2486
Simple MRI score to evaluate the effect of cerebral small vascular disease on the mental state of patients with hemodialysis1the First Affiliated Hospital of Dalian Medical University, Dalian, China, 2Philips Healthcare, Beijing, China
Synopsis
Keywords: Blood vessels, Neuroscience, Psychiatric Disorders
Hemodialysis(HD) can lead to hemodynamic changes and result in the occurrence of cerebral small vascular diseases(CSVD), which can cause changes in the mental state of patients. The objective of this study was to evaluate the effect of CSVD on the mental state of patients with hemodialysis by simple MRI score. Preliminary results show that HD is more likely to induce more serious CSVD and increase the prevalence of anxiety and depression, especially periventricular white matter hyperintensities (PVWMH) and cerebral microbleeds(CMB), which are closely related to the occurrence of anxiety and depression.Introduction
Hemodialysis (HD)-induced blood pressure fluctuations, myocardial dysfunction, and vascular dysfunction from inflammation and endotoxin release may lead to hemodynamic instability precipitating perfusion abnormalities and end-organ damage1. While, the brain, which is exposed to high blood volume and low resistance, is very sensitive to ischemic injury. Previous study have found that a higher prevalence and early-onset tendency of cerebral small vascular diseases (CSVD) in HD patients, especially for cerebral microbleeds (CMBs) and white matter hyperintensities (WMHs)2. CSVD is an important cause of stroke, dementia, and functional loss3. However, there are little studies about CSVD, anxiety and depression on HD patients. The purpose of our study was to evaluate the CSVD, cognitive, anxiety and depression in HD patients, so as to more comprehensively evaluate the impact of HD on patients.Methods
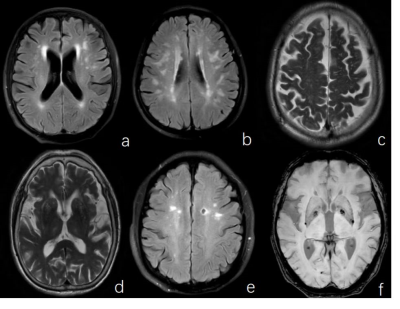
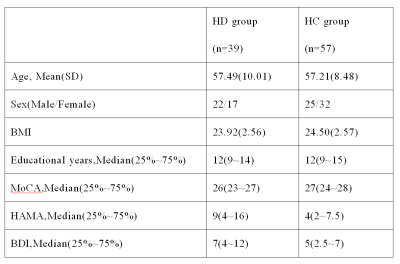
96 cases, whose age, gender, height, weight, BMI, educational level were matched, were included in this study: 39 cases with HD(17 females, 57.49±10.01 years) and 57 HC(32 females, 57.21±8.48 years). All participants completed the Montreal Cognitive Assessment (MoCA), Hamilton Anxiety Scale (HAMA) and Beck Depression Inventory (BDI), and underwent the 3.0 T MR scanning with 32-channel head coil (Ingenia CX, Philips Healthcare, the Netherlands). We evaluated the imaging findings of CSVD by T1W and T2W images. Refer to previous literature reports4-6, CSVD included PVWMH, DWMH, extensive perivascular space of centrum semiovale(C-EPVS) and basal ganglia region(B-EPVS), lacunes, CMBs, and then calculated the total burden of CSVD(TCSVD)(Fig 1). We used Nonparametric test to compare the difference of CSVDs and MoCA grade between HD group and HC group. We also used Chi-square test to compare the incidence of anxiety and depression between HD group and HC group. And then, we used Spearman correlation method to analyze the correlation between CSVD and cognition, anxiety and depression respectively. For all tests, a value of P<0.05 was considered to indicate statistical significance.Results
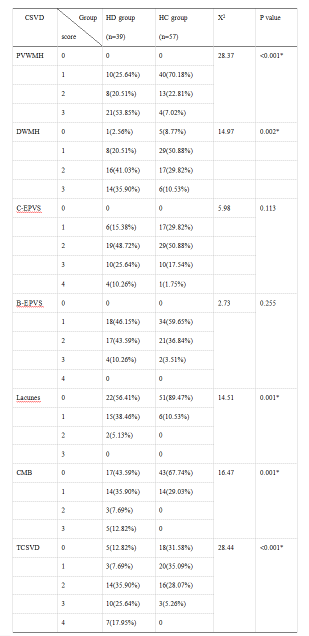
Demographic and clinical statistics are shown in Table 1. Compared with HC group, the PVWMH(χ2=28.37, P<0.001), DWMH(χ2=14.97, P=0.002), lacunes(χ2=5.101, P=0.024), CMB(χ2=5.101, P=0.024) and TCSVD(χ2=5.101, P=0.024) of HD group have statistical difference. While, there is no difference of C-EPVS and B-EPVS between HD group and HC group(P>0.05)(Tab 2). The MoCA grade has a decreasing trend in HD group(P=0.05). The anxiety occurrence rate of HD group(59%, 23/39) is higher than HC group(31.6%, 18/57) (χ2=7.103,P=0.008). The depression occurrence rate of HD group(23.1%, 9/39) was also higher than HC group(7.0%, 4/57)(χ2=5.101, P=0.024). In addition, our study found that DWMH was negatively correlated with MoCA score(r=-0.244, P=0.017), PVWMH was positively correlated with HAMA score(r=0.236, P=0.021), CMB was positively correlated with HAMA score(r=0.263, P=0.01) and BDI score(r=0.279, P=0.006).Discussion
In this study, compared with HC group, the CSVD had statistic difference, except EPVS (P<0.05). And the occurrence rate of PVWMH 3 score(21/39, 53.85%) and DWMH 2 score(8/39, 20.51%) were highest in HD group. While, the occurrence rate of PVWMH 2 score(13/39, 22.81%) and DWMH 1 score(29/57, 50.88%) were highest in HC group. The lacunes occurrence rate(17/39,43.59%; 6/57,10.53%) and CMB occurrence rate(22/39,56.41%;14/57,29.03%) were higher in HD group(P<0.05). Our study shows that HD patients are more likely to suffer from CSVD, and the degree is more serious than normal people. Besides, we found MoCA score of HD group(26, 23~27) had a lower trend than HC group(27, 24~28)(P=0.053). That means hemodialysis has the potential to reduce cognitive function in patients. And we also found MoCA score was negatively correlated with DWMH. Previous studies had shown that CSVD, especially lacunes and white matter hyperintensities, played an important role in the cognitive impairment of dialysis patients, and the cause of cognitive impairment in hematodialysis patients was cerebral ischemia1,7,8. Our study showed that it was due to the ischemia and hypoxia in deep white matter, that lead to cognitive impairment in HD patients. The effects of CMB on cognitive function have being debated. One study showed deep microbleeding was closely related to cognitive impairment9. But we did not find a correlation between CMB and cognitive function, which may be related to that we did not distinguish the location of CMB. At the same time, we found that CMB was positively correlated with the anxiety and depression. It may be related to the location of CMB, which needs to be further study. In addition, PVWMH was positively correlated with anxiety, while DWMH was not.Conclusion
The results of our study show that hemodialysis is more likely to induce more serious CSVD and increase the prevalence of anxiety and depression, especially PVWMH and CMB, which are closely related to the occurrence of anxiety and depression.Acknowledgements
No acknowledgement found.References
[1] Marants R, Qirjazi E, Grant CJ, et al. Renal perfusion during hemodialysis: Intradialytic blood flow decline and effects of dialysate cooling. J Am Soc Nephrol. 2019;30(6):1086–1095.
[2] Zheng K, Zhou YZ, Qian YJ, et al. Increased premature cerebral small vessel diseases in dialysis patients: A retrospective cross-sectional study.Nephron. 2021; 145(4):330-341.
[3] Pantoni L.Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010; 9(7): 689-701.
[4] Fazekas F, Chawluk JB, Alavi A, et al. MR signal abnormalities at 1.5 T in Alzheimer's dementia and normal aging. American journal of roentgenology. 1987; 149(2): 351-356.
[5] Koren-Morag N, Goldbourt U, Tanne D. Renal dysfunction and risk of ischemic stroke or TIA in patients with cardiovascular disease. Neurology. 2006; 67(2):224-228.
[6] Staals J, Makin SDJ, Doubal FN, et al. Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology. 2014; 83(14):1228-1234.
[7] Chai C, Wang ZY, Fan LL, et al. Increased number and distribution of cerebral microbleeds is a risk factor for cognitive dysfunction in hemodialysis patients: A longitudinal study. Medicine. 2016;95(12):e2974.
[8] Wolfgram DF. Intradialytic cerebral hypoperfusion as mechanism for cognitive impairment in patients on hemodialysis. J Am Soc Nephrol. 2019; 30(11): 2052-2058.
[9] Qian YJ, Zheng K, Wang HY, et al. Cerebral microbleeds and their influence on cognitive impairment in dialysis patients. 2021; 15(1): 85-95.
Figures