2463
Evaluation of the relationship between meniscal T2* metrics and tibial bone shape
Erin C Argentieri1, Kenneth Gao1, Valentina Pedoia1, Garry Gold2, Matthew F Koff3, Hollis G Potter3, and Sharmila Majumdar1
1Radiology, University of California San Francisco, San Francisco, CA, United States, 2Radiology, Stanford University, Stanford, CA, United States, 3Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States
1Radiology, University of California San Francisco, San Francisco, CA, United States, 2Radiology, Stanford University, Stanford, CA, United States, 3Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States
Synopsis
Keywords: Cartilage, MSK
Features of tibial bone morphology such as tibial slope and tibial spine volume have a significant impact on overall joint mechanics and, results of the current study indicate that these feature of tibial bone shape impact both medial and lateral meniscal T2* metrics.Introduction
Features of tibial bone morphology such as medial compartment slope and spine volume have a significant impact on overall joint mechanics and have been implicated as risk factors for sustaining non-contact ACL-injuries1,2. While previous studies found that meniscal T2* metrics prolong in the setting of degeneration3,4 and that qMRI metrics of articular cartilage are influenced by tibiofemoral bone morphology5, to date, no previous studies have attempted to evaluate the relationship between meniscal T2* metrics and tibial bone morphology. Therefore, the objective of this study was to determine the relationship between meniscal T2* metrics and tibial bone shape characterized via principle component analysis, with the hypothesis that tibial bone shape would be predictive of compartment and region specific meniscal T2* metrics.Methods
These data were collected as a part of a larger overall IRB-approved multi-institutional study within elite NCAA athletes. Clinical 3T MRIs were acquired on 39 knees (23 subjects) using an 8-channel phased array knee coil (Invivo). Medial and lateral menisci were manually segmented (MeVisLab) from three-dimensional, Cones UTE sequences (TEs: 5 echoes between 0.03-24ms, TR: 188ms, voxel size: 0.63x0.63x3mm3, RBW: ±83.3kHz, Flip-Angle: 16°). Mean and median meniscal T2* metrics were calculated via a mono-exponential fit of signal intensity to corresponding echo time (Matlab, Natick, MA). Segmentation of tibial bone was performed automatically via a fully convolutional neural network (V-Net) and were used to produce 3D triangulated meshes of tibial bone. The V-Net model achieved 0.98 ± 0.01 Dice Score coefficient in the unseen test set for tibia segmentation. Principal component analysis (PCA) was then performed to simplify the complexity of those surface data for interpretation/characterization over PC modes. 3D models for each of the modes were visualized for characterization using custom MeVisLab software (Figure 1). Statistical Analysis: Multiple linear regression and ANOVA analyses were performed to evaluate the influence of tibial bone shape (PC modes), BMI, and sex on compartment specific meniscal T2* metrics. Significance was set at p<0.05.Results
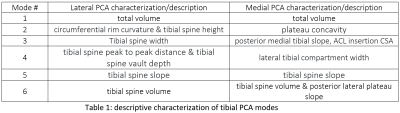
PCA Characterization: Percent variance captured by first 6 tibial modes: 83.3039% (Table 1; Figure 1) Lateral meniscus: Mean T2*: PCA-modes 1-6, and BMI combined to explain 35.77% of the variance in mean T2* metrics, and an ANOVA found that this effect was significantly different from zero, (p = .034, R2 = 0.36). Median T2*: PCA-modes 1-6, and BMI combined to explain 45.94% of the variance in median T2* metrics, and an ANOVA found that this effect was significantly different from zero, (p = .003, R2 = 0.46). Medial meniscus: Mean-T2*: PCA-modes 1-6 and BMI combined to explain 35.77% of the variance in mean T2* metrics explained 37.92% of the variance in mean T2* metrics (p = .022, R2 = 0.38). Median-T2*: BMI and PCA-modes 1-6 explained 49.11% of the variance in median T2*, and an ANOVA found that this effect was significant (p = .001, R2 = 0.49).Discussion
PCA-modes 1-6 and BMI significantly impacted both medial and lateral meniscal T2* metrics. Modes 2-6 largely characterized tibial spine morphology and compartment slope. Additionally, CSA of the distal ACL insertion on the anterior medial tibia was evident in PCA-mode 4 and related to medial meniscal T2* metrics within this cohort. Interestingly, medial meniscal T2* metrics were better explained by included PCA-modes as compared to lateral T2*, which may suggest that the features of joint morphology that are associated with ACL-injury risk (medial slope, medial spine volume, ACL-CSA)6,7,8 are also associated with acute meniscal injury or longitudinal meniscal degeneration. While the results of the current study are based on a population of young and elite athletes, tibial bone shape is a non-modifiable factor in joint biomechanics, which may suggest that these data could inform similar models across more heterogeneous cohorts.Conclusion
Evaluation of the relationship between meniscal T2* metrics and tibial PCA modes may allow for the development of individual risk equations for both acute meniscal injury as well as longitudinal degenerative processes.Acknowledgements
The authors acknowledge funding from the GE/NBA Research Consortium,and would like to thank all of the MRI techs and support staff at HSS for their assistance with this study.References
(1) Sturnick 2014; (2) Beynnon 2014; (3) Koff 2014; (4) Williams 2012, (5) Gao 2021 (6) Beynnon 2022 (7) Whitney 2014 (8) Vacek 2016
DOI: https://doi.org/10.58530/2023/2463