2458
Meniscus UTE-T2* Measured Prior to Anterior Cruciate Ligament Reconstruction Predicts Radiographic Osteoarthritis 11 Years Later1Orthopaedic Surgery, Stanford University, Stanford, CA, United States, 2Orthopaedic Surgery, University of Pittsburgh, Pittsburgh, PA, United States, 3Department of Radiology, New York University Grossman School of Medicine, New York, NY, United States, 4Department of Radiology, Stanford University, Stanford, CA, United States
Synopsis
Keywords: Osteoarthritis, Relaxometry, UTE-T2*, meniscus, radiography
This study examines whether compositional degeneration of the meniscus is a potential predictor of future radiographic knee OA. Mensical UTE-T2* maps acquired prior to anterior cruciate ligament reconstruction (ACLR) were compared to knee radiographs collected 11 years later in 11 ACLR patients. On average, pre-operative posterior medial and lateral meniscal UTE-T2* values were 39% and 33% higher in knees with KL grade ≥ 2 compared to knees with KL grades 0-1 at 11-year follow-up (p=0.016, 0.034). Thus, elevated meniscal UTE-T2* in the context of an ACLR knee may be a warning of increased risk for radiographic osteoarthritis many years later.PURPOSE
Although anterior cruciate ligament reconstruction (ACLR) restores knee stability following an ACL tear, approximately 50% of ACLR patients develop knee osteoarthritis (OA) within 10 to 15 years of injury.1; 2 ACL tears are often accompanied by trauma to the posteromedial and posterolateral menisci (pMM, pLM) which are the secondary restraints to anterior tibial translation and combined axial and rotary loads, respectively.3 Ultrashort echo time-enhanced T2* (UTE-T2* mapping) is sensitive to subsurface injury and degeneration of the pMM and pLM following ACL tear, even in the absence of frank meniscal tears or clinically detectable meniscus pathology.4; 5 However, the degree to which compositional changes of the menisci are associated with long-term knee OA has not been investigated. This study examines whether compositional degeneration of the meniscus is a potential predictor of future knee OA. We hypothesize that higher meniscal UTE-T2* values measured after ACL injury will be associated with a greater prevalence of radiographic OA6; 7 10+ years after ACLR.METHODS
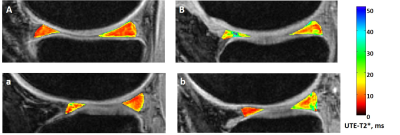
UTE-T2* relaxation was measured in the menisci of 30 ACL-deficient participants (17 females; mean age: 31 (SD: 9) years, mean BMI: 28 (SD: 6) kg/m2) within 40 days prior to reconstruction surgery. Radiographs of the lower limbs were obtained 10-12 years post-ACLR. Participants provided written consent for both the initial4 and follow-up IRB-approved studies. MRI T2* images were acquired with a 3-D AWSOS (Acquisition-Weighted Stack of Spirals)8 sequence using a 3T scanner (Siemens) and an 8-channel knee coil (Invivo, Gainsville, FL) at 11 TEs ranging 0.6-40 ms were collected as previously reported.4 Pixel-by-pixel mono-exponential T2* fits were generated with MRIMapper software (© Beth Israel Deaconess and MIT 2006). Two regions of interest (ROIs) were manually segmented on each of 2 single sections from the centers of the medial and lateral compartments of the knee to include the anterior and posterior horns of the medial and lateral menisci (aMM, pMM, aLM, pLM), Figure 1. Mean UTE-T2* values were averaged across all voxels within the ROI. Kellgren-Lawrence (KL)6 scoring of follow-up radiographs was performed by a musculoskeletal radiologist. Normality of all data sets was assessed by Shapiro-Wilk tests. UTE-T2* values in participants with x-ray scores KL 0-1 were compared to those of participants with KL scores ≥ 2 (definite osteophytes) with t-tests (or Mann-Whitney U tests). Statistical analyses were performed with SPSS (v25, IBM); significance was accepted for p < 0.05.RESULTS
UTE-T2* prediction of radiographic OA at 11 years post ACLR. Follow-up x-rays were collected in 11/30 participants at 11 years (11.4 (95%CI: 11.0, 11.8) years) after ACLR (6 females; mean age: 30 (SD: 11) years, mean BMI: 26 (SD: 5) kg/m2). Five participants were found to have radiographic OA (KL ≥ 2) of their ACLR knee, while 6 participants did not (KL 0-1). On average, pre-operative posterior medial and lateral meniscal UTE-T2* values were 39% and 33% higher in knees with KL grade ≥ 2 compared to knees with KL grades 0-1 at 11-year follow-up (p=0.016, 0.034), Figure 2. Neither age nor BMI differed by KL group (p>0.7). Medial meniscal tears were present at the time of ACLR in 3/5 participants with KL ≥ 2 and 1/6 participants with KL 0-1. Between ACLR and 11-yr follow-up, 2 participants, one in each KL group, reported re-injury to their ACLR knee but neither required additional surgery. Anterior medial and lateral meniscal UTE-T2* values did not differ by KL group (p>0.7).DISCUSSION
Meniscus UTE-T2* measured prior to ACLR predicted radiographic OA prevalence 11 years later in a small cohort of patients. Significantly elevated UTE-T2* values, indicating compositional degeneration of the subsurface substance4; 5; 10 of the posterior horns of both the medial and lateral menisci, were detected in knees demonstrating KL grade ≥ 2 compared to knees without radiographic evidence of OA. Development of radiographic OA following ACLR in knees with torn menisci is thought to be mediated by inadequate transmission of contact forces11; 12 and also by alteration of normal biologic activities within the menisci including upregulation of enzymes and inflammatory mediators capable of damaging the adjacent cartilage.13 While the mechanistic relationship between compositional meniscus degeneration, especially in grossly intact menisci, and the bony changes characteristic of radiographic OA remains to be elucidated, both mechanical and biologic factors may contribute to osseous remodeling.CONCLUSION
The results from this study support the interpretation of elevated meniscal UTE-T2* in the context of an ACLR knee as a sign of pre-OA and a warning of increased risk for radiographic osteoarthritis many years later.Acknowledgements
NIH RO1 AR052784 (PI – CR Chu) and DOD W81XWH-18-1-0590 (PI-CR Chu).References
1. Barenius B, Ponzer S, Shalabi A, et al. 2014. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med 42(5):1049-1057.
2. Lohmander LS, Englund PM, Dahl LL, et al. 2007. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 35(10):1756-1769.
3. Musahl V, Citak M, O'Loughlin PF, et al. 2010. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38(8):1591-1597.
4. Chu CR, Williams AA, West RV, et al. 2014. Quantitative Magnetic Resonance Imaging UTE-T2* Mapping of Cartilage and Meniscus Healing After Anatomic Anterior Cruciate Ligament Reconstruction. Am J Sports Med 42(8):1847-1856.
5. Williams A, Qian Y, Golla S, et al. 2012. UTE-T2 * mapping detects sub-clinical meniscus injury after anterior cruciate ligament tear. Osteoarthritis Cartilage 20(6):486-494.
6. Kellgren JH, Lawrence JS. 1957. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494-502.
7. Schiphof D, Boers M, Bierma-Zeinstra SM. 2008. Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis 67(7):1034-1036.
8. Qian Y, Boada FE. 2008. Acquisition-weighted stack of spirals for fast high-resolution three-dimensional ultra-short echo time MR imaging. Magn Reson Med 60(1):135-145.
9. Brown G, Amendola A. 2012. Radiographic Evaluation and Preoperative Planning for High Tibial Osteotomies. Oper Tech Sports Med 20:93-102.
10. Juras V, Apprich S, Zbyn S, et al. 2014. Quantitative MRI analysis of menisci using biexponential T2* fitting with a variable echo time sequence. Magn Reson Med 71(3):1015-1023.
11. Jones MH, Spindler KP. 2017. Risk factors for radiographic joint space narrowing and patient reported outcomes of post-traumatic osteoarthritis after ACL reconstruction: Data from the MOON cohort. J Orthop Res 35(7):1366-1374.
12. Nordenvall R, Bahmanyar S, Adami J, et al. 2014. Cruciate ligament reconstruction and risk of knee osteoarthritis: the association between cruciate ligament injury and post-traumatic osteoarthritis. a population based nationwide study in Sweden, 1987-2009. PLoS One 9(8):e104681.
13. Riordan EA, Little C, Hunter D. 2014. Pathogenesis of post-traumatic OA with a view to intervention. Best Pract Res Clin Rheumatol 28(1):17-30.
Figures