2453
Associations between Weight Change, Knee Subcutaneous Fat and Cartilage Thickness: 4-Year Data from the OAI1Department of Radiology and Biomedical Imaging, UCSF, San Francisco, CA, United States, 2Department of Epidemiology and Biostatistics, UCSF, San Francisco, CA, United States, 3Department of Rheumatology, UC Davis, Davis, CA, United States
Synopsis
Keywords: Osteoarthritis, Cartilage
This study assessed the relationship between 4-year changes in: (1) body weight and outcomes of joint-adjacent subcutaneous fat (SCF) and cartilage thickness, and (2) joint-adjacent SCF and knee cartilage thickness. A total of 399 individuals from the Osteoarthritis Initiative with >10% weight gain and >-10% weight loss over 4 years were compared with controls with less than 3% weight change. Weight gain and loss were associated with increases, and decreases, respectively in joint-adjacent SCF. Increases in SCF adjacent to the medial femur were associated with decreases in average cartilage thickness and in several medial and lateral locations in the knee.
Objective:
Osteoarthritis (OA) affects over 32.5 million adults in the US and is the most common cause of disability1. Obesity is a significant risk factor for OA, contributing to disease progression through both systemic inflammatory effects and localized increases in joint-adjacent adipose tissue. Recently, joint-adjacent subcutaneous fat (SCF) has gained interest as an independent risk factor of OA progression2, and studies using MR imaging have reported associations between SCF and knee cartilage morphology and biochemical composition3. This study focuses on the effects of weight change (weight loss and weight gain) on change in joint-adjacent SCF over 4 years. The purpose of this study was to assess the relationship between 4-year changes in: (1) body weight and outcomes of joint-adjacent subcutaneous fat (SCF) and cartilage thickness, and (2) joint-adjacent SCF and knee cartilage thickness.Methods:
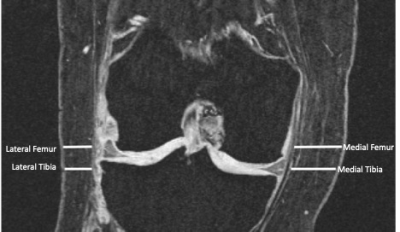
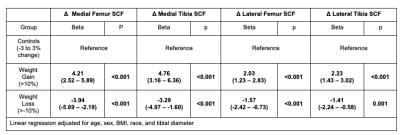
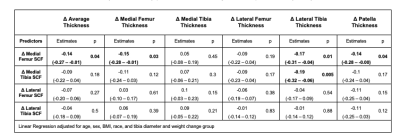
A total of 399 Individuals from the Osteoarthritis Initiative (OAI) with >10% weight gain (n=100) and >10% weight loss (n=100) over 4 years were compared to an age, gender, BMI, Kellgren-Lawrence (KL) grade-matched control cohort with less than 3% change in weight (n=199). MR imaging was performed using 3T MRI scanners (Trio, Siemens, Erlangen, Germany) at four centers as part of the imaging OAI protocol at baseline and after 4 years. The following sequences of the right knee were analyzed in this study: 1) coronal 3D fast low angle shot with water excitation (FLASH WE) [7.57 ms/20 ms; 0.313 mm × 0.313 mm; 160 mm; 1.5 mm; 0 mm] and 2) sagittal 3D dual-echo steady state sequence with water excitation (DESS WE) [4.7 ms/16.3 ms; 0.365 mm × 0.456 mm; 140 mm; 1.5 mm; 0 mm] with axial and coronal reformations. Joint-adjacent SCF was measured on coronal 3D FLASH WE MRI sequence at four locations on the medial and lateral sides of the knee joint (Figure 1) at baseline and 4-year follow-up. Cartilage thickness was measured on the 3D DESS sequence using a fully-automatic, deep learning method that has been previously developed and validated by our group4. Cartilage thickness was quantified in five knee regions (medial/lateral tibia and medial/lateral femur and patella, and the average thickness in all regions) at baseline and 4-year follow-up. Changes in SCF and cartilage thickness, respectively, were defined by subtracting the baseline measurement from the 4-year follow-up measurement. Linear regression models were used to evaluate the associations between (1) weight change group and 4-year changes in both knee SCF and cartilage thickness and (2) 4-year changes in knee SCF and 4-year changes in cartilage thickness. For analysis (2), the beta coefficients represent the standard deviation change of the outcome, per standard deviation change of the predictor. All analyses were adjusted for age, sex, BMI, and tibial diameter (and weight change group in analysis (2)).Results:
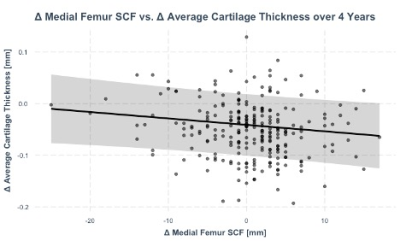
There were no significant differences (p>0.05) in age, BMI, sex, and KL grade between the weight gain, weight loss, and control groups at baseline. Individuals who gained weight over 4-years had significantly greater increases in joint-adjacent SCF (beta range, medial/lateral joint sides: 2.2mm to 4.2mm, p<0.001) than controls after 4 years, while individuals who lost weight had significantly greater decreases in joint-adjacent SCF than controls (beta range: -1.4mm- -3.9mm, p<0.001, Table 1). No statistically significant (p>0.05) associations were found between weight change and cartilage thickness change over 4 years. However, increases in joint-adjacent SCF over 4-years were significantly associated with decreases in cartilage thickness (1 SD increase in medial femur SCF was associated with 0.14 SD decrease in average in thickness, p=0.04), Figure 1 and Table 2. In addition to average cartilage thickness, increases in medial femur SCF were associated with decreases in medial femur cartilage thickness (coeff_standardized.=-1.5, p=0.03), lateral tibia thickness (coeff_standardized.=-0.17, p=0.01), and patella thickness (coeff_standardized.=-0.14, p=0.04).Conclusion:
Weight change was significantly associated with joint-adjacent SCF independent of BMI, but not with cartilage thickness. However, 4-year increases in joint-adjacent SCF were associated with decreases in cartilage thickness independent of BMI. Thus, cartilage thickness changes may be more sensitive to changes in joint-adjacent SCF rather than changes in BMI, potentially due to the localized nature of joint-adjacent SCF measurements. Increases in SCF may also be better predictors of cartilage loss than increases in BMI.Acknowledgements
This study was funded by NIH R01-AR064771, NIH R01-AR078917 and R01-AG070647 The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health.References
1. Initiative, U. B. a. J. The Burden of Musculoskeletal Diseases in the United States (BMUS). https://www.boneandjointburden.org/fourth-edition/iiib10/osteoarthritis (accessed September 29).
2. Chang, J.; Liao, Z.; Lu, M.; Meng, T.; Han, W.; Ding, C., Systemic and local adipose tissue in knee osteoarthritis. Osteoarthritis Cartilage 2018, 26 (7), 864-871.
3. Bodden, J.; Ok, A. H.; Joseph, G. B.; Nevitt, M. C.; McCulloch, C. E.; Lane, N. E.; Link, T. M., Joint-adjacent Adipose Tissue by MRI is Associated With Prevalence and Progression of Knee Degenerative Changes: Data from the Osteoarthritis Initiative. J Magn Reson Imaging 2021, 54 (1), 155-165.
4. Iriondo, C.; Liu, F.; Caliva, F.; Kamat, S.; Majumdar, S.; Pedoia, V., Towards understanding mechanistic subgroups of osteoarthritis: 8-year cartilage thickness trajectory analysis. J Orthop Res 2021, 39 (6), 1305-1317.
Figures