2447
Lower abdominal adipose result in higher postoperative early recurrence in HCC patients with HBV1Qilu Hospital of Shandong University, Jinan, China
Synopsis
Keywords: Liver, Cancer
Problem: To investigate the incremental value of abdominal adipose to identify postoperative early recurrence in hepatitis B virus (HBV) patients with hepatocellular carcinoma (HCC). Methods: Visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) areas were measured in the third lumbar vertebra plane of T1-weighted images. Results: HCC with microvascular invasion, portal invasion, and satellite nodules patients had lower VAT and SAT areas. VAT and SAT areas were important risk factors for early recurrence. Conclusions: Decreased VAT and SAT areas have significant impact regarding the postoperative early recurrence and poorer HCC biological behavior in HBV patients with HCC.
Introduction
Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related death, in which chronic infection with hepatitis B virus (HBV) is the largest etiologic risk factor for HCC among the Chinese population1, 2. Traditionally, obesity is an important risk factor for poor prognosis of HCC. Obesity and excess adipocytes can induce to a low-grade inflammatory disease and make the liver susceptible to a pro-tumor environment3. As a result, this environment may be exacerbated by HBV infection, leading to a more aggressive disease state. However, there is growing evidence that obese/overweight cancer patients have a lower mortality rate than normal weight patients, which is known as the "obesity paradox"4, 5. A recent study showed that HCC patients with higher body mass index (BMI) had higher overall survival compared to those with lower BMI6, and Okamura et al.7 investigated that low BMI was an important prognostic factor for low HCC overall survival. Nevertheless, BMI is incapable to distinguish adipose from muscular tissue and display fat distribution8, which may be more important for the prognosis of HCC patients9. MRI has been widely used for preoperative imaging evaluation of HCC10, 11, which have been shown to be associated with pathological features and prognosis of HCC. In the meantime, MR and CT are the gold standard method for different adipose regions quantification. And MR is recognized as superior to CT because of its accuracy, non-invasiveness and lack of radiation. But the correlation of abdominal fat MR features with the biological behavior of HCC is currently not well explained. Whether abdominal fat MR features have incremental value for HCC prognosis in addition to traditional HCC MRI features has not been well characterized. The aim of this study was to investigate the incremental value of abdominal adipose to identify postoperative early recurrence in HBV patients with HCC.Methods
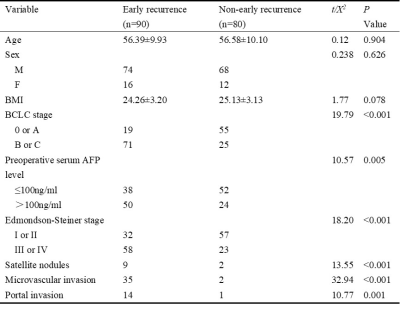
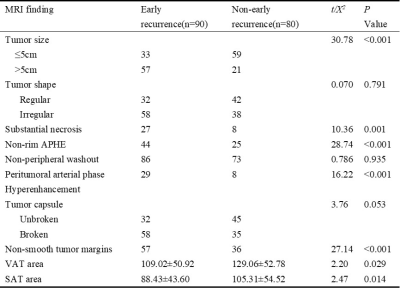
170 HBV with HCC patients confirmed by surgical pathology who underwent preoperative multiparametric MRI between January 2015 and January 2019 were enrolled in this retrospective study. The preoperative MRI characteristics were evaluated including tumor size, tumor shape, substantial necrosis, non-rim arterial phase hyperintensity, non-peripheral washout, peritumoral arterial phase hyperenhancement, tumor capsule, and non-smooth tumor margins. Visceral adipose tissue (VAT) was defined as intra-abdominal fat bound by parietal peritoneum or transverse fascia12. Subcutaneous adipose tissue (SAT) was defined as fat on the surface of abdominal and back muscles13. VAT area and SAT area were measured in the third lumbar vertebra plane of T1-weighted images using Slice-O-Matic 5.0 software (Tomovision, Magog, Canada). The differences in VAT and SAT distribution between various HCC biological behavior groups were compared. Univariate and multivariate logistic regression was used to analyze the risk factors for postoperative early recurrence.Results
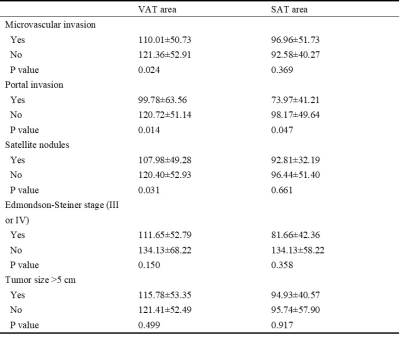
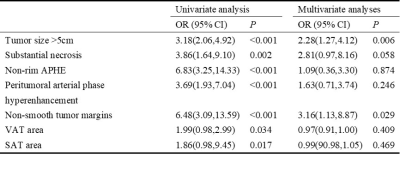
A total of 170 HBV with HCC patients (mean age 56.3 years, range 30-79 years, 142 men) underwent preoperative MRI were enrolled. Of the 170 HCC cases, 90 (52.94%) had early recurrence and 80 (47.06%) had non-early recurrence. Patients in the early recurrence group had lower SAT area (P=0.014) and VAT area (P=0.029). HCC with microvascular invasion, portal invasion, and satellite nodules patients had lower VAT area than without patients (P=0.024, 0.014, 0.031, respectively). HCC with portal invasion patients also had lower SAT area than without patients(P=0.047). In univariate logistic analysis, tumor size >5cm, substantial necrosis, non-rim APHE, peritumoral arterial phase hyperenhancement, non-smooth tumor margins, VAT and SAT area were important risk factors for early recurrence in HBV patients with HCC (P<0.05). In multivariate logistic analysis, tumor size >5cm (OR:2.28, 95%CI:1.27,4.12, P=0.006) and non-smooth tumor margins (OR:3.16, 95%CI:1.13,8.87, P=0.029) were independent risk factors for postoperative early recurrence in HBV patients with HCC.Discussion
This study for the first time showed that lower SAT and VAT areas were associated with poor biological behavior and postoperative early recurrence in HCC with combined HBV. This may be related to the following mechanisms. Firstly, this might be due to the effect of various adipokines secreted by VAT on living malignant cells maintained around the coagulation zone, which was proposed in Takaaki Higashi et al.14 study. Secondly, patients with lower abdominal fat were commonly in a more vulnerable immunological state and more susceptible to malignancies7. Thirdly, patients suffering from HBV are in an inflammatory state and deplete nutritional reserves. Abdominal fat may be linked to the nutritional status of HCC patients and influence the prognostic outcome6. Besides, there are differences between SAT and VAT in anatomical, cellular, and physiological. VAT adipocytes are more metabolically active and more sensitive to lipolysis15. In our study, we found a more pronounced reduction in VAT area in patients with poorer biological behavior HCC than SAT. The specific mechanisms behind VAT and SAT in biological behavior and HCC prognosis need to be further confirmed by basic studies.Conclusions
Decreased VAT and SAT areas have significant impact regarding the postoperative early recurrence and poorer HCC biological behavior in HBV patients with HCC. It is necessary to concern the HCC patients with significantly low VAT and SAT area in order to adjust treatment and follow-up.Acknowledgements
None.References
1. D'souza S, Lau KC, Coffin CS, et al. Molecular mechanisms of viral hepatitis induced hepatocellular carcinoma. World J Gastroenterol. 2020;26(38):5759-5783.
2. Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379(9822):1245-1255.
3. Zhao J, Lawless MW. Stop feeding cancer: pro-inflammatory role of visceral adiposity in liver cancer. Cytokine. 2013;64(3):626-637.
4. Curcic IB, Berkovic MC, Kuna L, et al. Obesity Paradox in Chronic Liver Diseases: Product of Bias or a Real Thing?. J Clin Transl Hepatol. 2019;7(3):275-279.
5. Lennon H, Sperrin M, Badrick E, et al. The Obesity Paradox in Cancer: a Review. Curr Oncol Rep. 2016;18(9):56.
6. Li Q, Xing H, Liu D, et al. Negative impact of low body mass index on liver cirrhosis patients with hepatocellular carcinoma. World J Surg Oncol. 2015;13:294.
7. Okamura Y, Maeda A, Matsunaga K, et al. Negative impact of low body mass index on surgical outcomes after hepatectomy for hepatocellular carcinoma. J Hepatobiliary Pancreat Sci. 2012;19(4):449-457.
8. Grundy SM, Brewer HB Jr, Cleeman JI, et al. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Arterioscler Thromb Vasc Biol. 2004;24(2):e13-e18.
9. Fujiwara N, Nakagawa H, Kudo Y, et al. Sarcopenia, intramuscular fat deposition, and visceral adiposity independently predict the outcomes of hepatocellular carcinoma. J Hepatol. 2015;63(1):131-140.
10. Chong H, Gong Y, Pan X, et al. Peritumoral Dilation Radiomics of Gadoxetate Disodium-Enhanced MRI Excellently Predicts Early Recurrence of Hepatocellular Carcinoma without Macrovascular Invasion After Hepatectomy. J Hepatocell Carcinoma. 2021;8:545-563.
11. Hectors SJ, Lewis S, Besa C, et al. MRI radiomics features predict immuno-oncological characteristics of hepatocellular carcinoma. Eur Radiol. 2020;30(7):3759-3769.
12. Tang L, Zhang F, Tong N. The association of visceral adipose tissue and subcutaneous adipose tissue with metabolic risk factors in a large population of Chinese adults. Clin Endocrinol (Oxf). 2016;85(1):46-53.
13. Tirkes T, Jeon CY, Li L, et al. Association of Pancreatic Steatosis With Chronic Pancreatitis, Obesity, and Type 2 Diabetes Mellitus. Pancreas. 2019;48(3):420-426.
14. Higashi T, Hayashi H, Kaida T, et al. Prognostic Impact of Visceral Fat Amount and Branched-Chain Amino Acids (BCAA) in Hepatocellular Carcinoma. Ann Surg Oncol. 2015;22 Suppl 3:S1041-S1047.
15. Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev. 2010;11(1):11-18.
Figures