2442
Active Breathing Guidance for T2-weighted liver MRI sequences: a novel in-bore solution for image quality and efficiency improvement
Narine Mesropyan1, Christoph Katemann2, Annerieke Heuvelink-Marck2, Alexander Isaak1, Dmitrij Kravchenko1, Leon Bischoff1, Ad Denissen2, Claus Christian Pieper1, Daniel Kuetting 1, Ulrike Attenberger1, and Julian Luetkens1
1Department of Diagnostic and Interventional Radiology, University Hospital Bonn, Bonn, Germany, 2Philips Healthcare, Philips Healthcare, Hamburg, Germany
1Department of Diagnostic and Interventional Radiology, University Hospital Bonn, Bonn, Germany, 2Philips Healthcare, Philips Healthcare, Hamburg, Germany
Synopsis
Keywords: Liver, Artifacts
Breathing artifacts in liver MRI lead to impaired image quality, decreased diagnostic confidence, and, as a consequence, longer acquisition times or repetitive examinations. To improve the image quality and scan efficiency we integrated a newly developed in-bore breathing guidance application for T2 weighted sequences with propeller acquisition (MultiVaneXD) (T2BG) and compared it to a conventional free-breathing acquisition method (T2conv). Our study results suggest that an active breathing guidance for T2w liver MRI sequences significantly reduces breathing artifacts and total scan times by 21% while maintaining high image quality.Introduction
Liver disease is a global burden with a growing incidence and prevalence1. Recent improvements in MRI techniques allow for non-invasive comprehensive assessment and monitoring of liver disease2. However, breathing artifacts are frequent in liver MRI and can lead to impaired image quality, decreased diagnostic confidence, and as a consequence, longer scanning times3. This is of clinical importance, especially in patients with irregular breathing patterns, comorbidities, and anxiety. Therefore, this study aimed to evaluate the image quality of a standard T2w sequence with propeller acquisition (MultiVaneXD) using a newly developed in-bore breathing guidance (T2BG) application in comparison to a conventional free-breathing acquisition (T2conv). Breathing guidance software was developed to improve the scan efficiency, image quality, and patient experience by guiding patients` breathing in a personalized, adaptive manner to a predefined target pattern during MRI examination.
Material and Methods
The institutional review committee approved this prospective study and all subjects gave written consent prior to MRI examination. Patients with clinical indications to liver MRI, who underwent examination at 3T MRI were consecutively included in this study. MRI protocol included a T2conv followed by a T2BG. For the active breathing guidance, a pre-clinical software was installed on the scanner. Prior to the scan session, each patient received short video instruction about the MRI with breathing guidance. Suitable parameters for desired breathing pattern for T2BG were set individually for each patient based on the patient`s physical respiratory ability and adaptivity. Artifacts, sharpness, lesion conspicuity, and overall image quality were assessed using a Likert grading scale from 1 (non-diagnostic) to 5 (excellent). Additionally, scanning time, time of repetition (TR), contrast-to-noise (CNR: SIliver-SInoise/SDnoise), and signal-to-noise ratio (SNR: SIliver/SInoise) were analyzed. Measurements were performed in consensus by two experienced board-certified radiologists. Paired t-test and Wilcoxon test were used for statistical analysis.Results
35 patients (51±16 years; 12 female) were included. T2BG showed significantly less artefacts (4.5±0.7 vs.4.0±0.9, P<0.001) and better sharpness (4.7±0.6, P=0.003) compared to T2conv. Overall image quality (4.5±0.8 vs. 4.3±0.9, P=0.062) and lesion conspicuity (4.7±0.6 vs. 4.6±0.6, P=0.5) were similar for both T2BG and T2conv. T2BG had significantly longer TR (3608±667ms vs. 2244±384ms; P<0001). Sequence scan time was shorter with T2BG (4.1±1.2min vs. 5.2±1.2min; P=0.041), with a reduction of scan time by 21%. SNR (70.2±40.7 vs. 67.1±36.2, P=0.624) and CNR (68.2±40.4 vs. 65.2±35.9, P=0.623) were similar for both imaging approaches.Discussion
Despite improvements in MRI techniques, it remains very sensitive to breathing artifacts. The implementation of the breathing guidance application may overcome these limitations by ensuring the patient has an appropriate individual breathing pattern allowing for the reduction of breathing artifacts and improved image quality during a shorter scan time. Our study results demonstrated that using breathing guidance, especially artifacts were reduced and sharpness improved. More importantly, a significant reduction of acquisition times was achieved without affecting quantitative (SNR and CNR) and qualitative (overall image quality and lesion conspicuity) parameters of image quality. Further prospective studies on a larger patient population, also in combination with other breathing artifacts sensitive sequences (e.g., diffusion-weighted imaging, MR-cholangiopancreatography) have to be performed to evaluate the potential of breathing guidance application in clinical routine.Conclusion
Our study results indicate that active breathing guidance for T2w liver MRI sequences lead to the significant reduction of breathing artifacts by significantly shorter total scan times while maintaining high image quality. The application of an active visualized breathing guidance for breathing sensitive MRI sequences could improve scan efficiency, image quality, diagnostic confidence, and possibly patient experience.Acknowledgements
The present work was supported by Philips HealthcareReferences
References
1. Asrani SK, Devarbhavi H, Eaton J, Kamath PS (2019) Burden of liver diseases in the world. J Hepatol 70(1):151–71.
2. van Beers BE, Daire J-L, Garteiser P (2015) New imaging techniques for liver diseases. J Hepatol 62(3):690–700.
3. Kim BS, Lee KR, Goh MJ (2014) New imaging strategies using a motion-resistant liver sequence in uncooperative patients. Biomed Res Int 2014:142658.
Figures
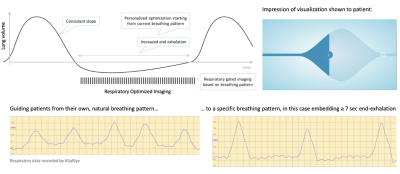
Breathing Guidance application – an in-bore solution guiding patients towards a personalized breathing pattern in order to improve scan efficiency, image quality and patient experience
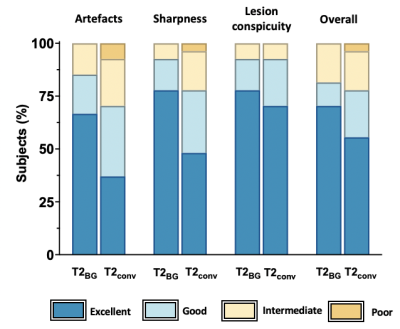
Subjective image quality assessment. Bar plots of image quality scores of T2 MVXD with the breathing guidance (T2BG ) and conventional T2 MVXD (T2conv) using 5-point Likert grading scale
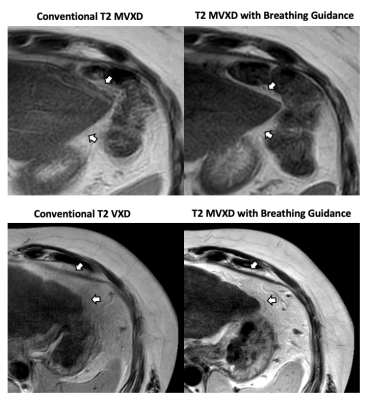
Representative images of two patients who underwent liver MRI with T2conv followed by T2BG. T2BG provides high image quality with significant improvement of sharpness and reduction of breathing artefacts during shorter scan time
DOI: https://doi.org/10.58530/2023/2442