2356
Reducing femoral flow artefacts in radial MR Fingerprinting: A comparison of two methods applied to prostate imaging1Department of Circulation and Medical Imaging, Norwegian University of Science and Technology, Trondheim, Norway, 2Department of Radiology and Nuclear Medicine, St. Olavs hospital, Trondheim University Hospital, Trondheim, Norway, 3Centre for Advanced Imaging, The University of Queensland, Brisbane, Australia
Synopsis
Keywords: MR Fingerprinting/Synthetic MR, Artifacts
High acceleration factors in radial magnetic resonance fingerprinting (MRF) of the prostate lead to strong streaking artefacts from flow in the femoral blood vessels, distorting quantitative T1 and T2 measurements. We here compare two approaches to mitigate these artefacts, namely incorporating regional saturation bands in the MRF sequence (Sat-MRF) or applying region-optimized virtual coils to suppress signal from select spatial regions before image reconstruction (ROVir-MRF). Results from seven asymptomatic volunteers show that both methods efficiently reduce signal in the region of the femoral vessels, but there are differences in retained prostate signal to noise ratio and sensitivity to T1.
Introduction
Mapping of both T1 and T2 relaxation times shows promise for discriminating prostate cancer from benign prostatic tissue1,2, but is not routinely performed because classical mapping sequences have long acquisition times. Magnetic resonance fingerprinting (MRF) aims to facilitate quantitative T1 and T2 mapping in a clinically viable time3, and has been used in combination with apparent diffusion coefficient maps to characterize prostate tissue4.One of the key features of MRF is the use of incoherent undersampling in combination with a model-based reconstruction5. In radial MRF of the prostate high acceleration factors lead to strong streaking artefacts from blood flowing in the femoral vessels, distorting quantitative measurements in the prostate6.
This work compares two approaches to mitigate femoral flow streaking artefacts in prostate MRF. 1) A radial MRF sequence including saturation bands covering the femoral vessels7. 2) Region-optimized virtual (ROVir) coils to suppress signal from select spatial regions8. The comparison is done by assessing the methods’ ability to suppress streaking artefacts while retaining signal to noise ratio (SNR) and sensitivity to T1 and T2.
Methods
Two MRF sequences were used. The original pulse sequence design9, hereafter referred to as MRF, and a modified version including regional saturation blocks (two every 25th repetition time)7, hereafter referred to as Sat-MRF. These saturation bands were placed to cover the femoral vessels to suppress the bright signal from the blood flow (Fig 1). All data was reconstructed and analysed in Matlab (MathWorks, Natick, MA, USA), as described by Ma et al3 and Cloos et al5,9.Seven asymptomatic volunteers (median age: 31, range: 25-33 years) were imaged with both MRF and Sat-MRF, using four shots (resolution matrix 208x208, field of view 240x240 mm, slice thickness 5 mm, 8 slices, acquisition time 4:49 for MRF and 5:06 for Sat-MRF). A vessel scout scan was performed to guide the positioning of the saturation bands for Sat-MRF (acquisition time 0:57). The data was collected at St. Olavs hospital, Trondheim University Hospital, Norway on a Magnetom Skyra 3T MRI system (Siemens, Erlangen, Germany). The Regional Committee for Medical and Health Research Ethics approved the study, and all volunteers signed informed consents prior to recruitment (REC identifier #218665).
The ROVir framework8 was applied only on the unsaturated MRF in an automated pipeline (Fig 2) designed to maximize signal energy in the prostate while minimizing signal energy in the femoral vessels. The virtual coils were optimized for slice four and applied on all slices. The region of interest was a circle placed in the centre of the image (radius of 30 mm), expected to contain the prostate. The femoral vessels were automatically detected using the two-stage circular Hough transform (imfindcircles in Matlab) on the root-sum-of-square image of the coil images. To increase accuracy of imfindcircles, the image was five times enlarged and cropped to remove the oversampling and the posterior half of the image. The four circles with highest metric were dilated with 3 pixels and used joint as region of interference. Retained interference signal energy in the virtual coils was calculated8, and selected virtual coils were removed from reconstruction to retain less than 5% of the interference.
The prostate was manually segmented on the MRF images by a researcher with three years of experience with prostate MRI (K.I.S.), and mean and standard deviation of prostate T1 and T2 were calculated for all volunteers. The B1-weighted prostate SNR was calculated10, where SNR relative to MRF was reported for Sat-MRF and ROVir-MRF.
Results and discussion
Both ROVir-MRF and Sat-MRF visibly reduce signal in the region of the femoral vessels (Fig 3). The streak pattern in the B1+ and T2 ROVir-MRF difference maps show that the femoral flow artefact is reduced, and the Sat-MRF difference maps show that the saturation bands effectively suppress signal from the region of the femoral vessels. ROVir-MRF and MRF are perfectly co-registered as they are reconstructed from the same acquisition, while Sat-MRF is reconstructed from a separate acquisition, possibly explaining the less apparent streaks from the femoral vessels in these difference maps.Although ROVir-MRF accurately removes signal from the femoral vessels, it also sacrifices some signal in the prostate. Fig 4 suggests that prostate SNR increases for Sat-MRF as compared to MRF, while ROVir-MRF displays a wider range of relative prostate SNR values.
Fig 5 shows that the average prostate T2 is similar for all methods, whereas T1 appears to decrease for Sat-MRF. Implementation of saturation bands in Sat-MRF leads to modifications in the dictionary matching procedure, possibly causing this bias. One advantage of ROVir-MRF is that it does not change the sequence, and maintain sensitivity to long T2s.
Neither of the approaches lead to significant increases in acquisition or post-processing time. However, Sat-MRF requires an additional vessel scout scan to place the saturation bands, while ROVir-MRF requires no additional user input in acquisition or post-processing. ROVir-MRF can also be applied to existing data if the raw data is still available.
Conclusion
Both Sat-MRF and ROVir-MRF can be used to reduce femoral flow streak artefacts from radial MRF images of the prostate. ROVir-MRF can be applied on existing data without changing the sensitivity of the sequence, while Sat-MRF appears to yield higher prostate SNR.Acknowledgements
No acknowledgement found.References
1. Baur, ADJ et al. Evaluation of T1 relaxation time in prostate cancer and benign prostate tissue using a Modified Look-Locker inversion recovery sequence. Sci Rep, 2020;10(1):1-8
2. Schieda N, Lim CS, Zabihollahy F, et al. Quantitative Prostate MRI. J Magn Reson Imaging, 2021; 53(6): 1632–1645.
3. Ma D, Gulani V, Seiberlich N, et al. Magnetic resonance fingerprinting. Nature, 2013; 495(7440): 187–192
4. Lo WC, Panda A, Jiang Y, Ahad J, Gulani V, Seiberlich N. MR fingerprinting of the prostate. Magn Reson Mater Phy, 2022;35(4)
5. Cloos MA, Knoll F, Zhao T, et al. Multiparametric imaging with heterogeneous radiofrequency fields. Nat Commun, 2016;7(1): 12445.
6. Sørland, KI et al. Reducing streak artefacts in radial MR fingerprinting of the prostate through automated channel removal. ISMRM Annual Meeting Proceedings, London 2022.
7. Trimble, CG et al. Incorporating saturation bands into MR Fingerprinting reduces streaking artefacts. ISMRM Annual Meeting Proceedings, London 2022.
8. Kim D, Cauley SF, Nayak KS, Leahy RM, Haldar JP. Region-optimized virtual (ROVir) coils: Localization and/or suppression of spatial regions using sensor-domain beamforming. Magn Reason Med, 2021; 86(1): 197–212
9. Cloos MA, Assländer J, Abbas B, et al. Rapid Radial T1 and T2 Mapping of the Hip Articular Cartilage With Magnetic Resonance Fingerprinting. J Magn Reson Imaging, 2019; 50(3): 810–815
10. Kellman P, McVeigh ER. Image Reconstruction in SNR Units: A General Method for SNR Measurement. Magn Reson Med, 2005; 54(6)
Figures
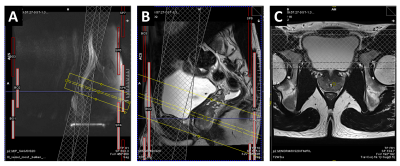
Figure 1: Placement of the saturation bands for Sat-MRF in an asymptomatic volunteer. A vessel scout scan (A) aids the placement of the two saturation slabs (in checkered grey), with the aim of suppressing as much of the blood-flow signal as possible without covering the prostate. The prostate is shown in the sagittal (B) and transversal (C) T2-weighted image, where the yellow box is the field of view for the MRF images.
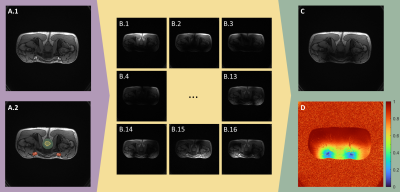
Figure 2: Automated region-optimized virtual (ROVir) coils pipeline for prostate MRF. A) Root sum of square (RSS) of all coil images without (A.1) and with (A.2) segmentations. Red: automated segmentation of the femoral vessels, green: central circle expected to contain the prostate, yellow: manual prostate segmentation. B) ROVir coil images for virtual coils 1-4 and 13-16. More than 95% of the interference signal within the red segmentation is located in the final two coils. C) RSS of the ROVir coil images after excluding coils 15-16. D) Percentage of retained signal in C relative to A.

Figure 3: MRF, ROVir-MRF and Sat-MRF maps of one asymptomatic volunteer reconstructed with two shots. The difference maps show difference to the MRF sequence. Proton density (PD) maps are scaled [0, 0.3 a.u.] with difference map [-0.2 a.u., 0.2 a.u.], B1+ scaled [0, 90◦] with difference map [-20◦, 20◦], T1 scaled [0, 3 s] with difference [-0.3 s, 0.3 s] and T2 scaled [0, 250 ms] with difference map [-20 ms, 20 ms]. Manual prostate segmentation in yellow.
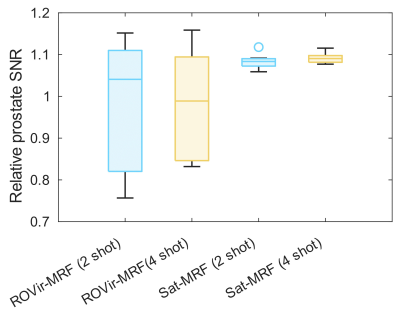

Figure 5: Box plots of the patient-wise mean T1 and T2 in the prostate, and the patient-wise standard deviation (STD) of T1 and T2 in the prostate. MRF, Sat-MRF and ROVir-MRF were reconstructed with either two or four shots.