2330
MR multitasking-based dynamic imaging forcerebrovascular evaluation (MT-DICE) in brain tumors1Radiology, Keck School of Medicine of USC, Los Angeles, CA, United States, 2Radiation Oncology, Keck School of Medicine of USC, Los Angeles, CA, United States, 3Cedars-Sinai Medical Center, Los Angeles, CA, United States, 4Viterbi School of Engineering, University of Southern California, Los Angeles, CA, United States
Synopsis
Keywords: Tumors, DSC & DCE Perfusion
Brain tumors represent a great therapeutic challenge and tend to impact blood brain barrier (BBB) integrity, angiogenesis, and vascularity. Dynamic contrast-enhanced (DCE) MRI is widely used to quantify BBB permeability and dynamic susceptibility contrast MRI (DSC) is used to quantify cerebral perfusion. We incorporated the newly developed MR multitasking-based dynamic imaging for cerebrovascular evaluation (MT-DICE) technique to achieve simultaneous DCE and DSC acquisition with a single-dose injection. MT-DICE could quantify DCE and DSC parameters with good inter-reader agreement in patients with brain tumors. The intratumoral enhanced region showed more severe BBB disruption and higher perfusion than the peritumoral T2-hyperintense regions.Introduction
Brain tumors tend to impact blood brain barrier (BBB) integrity, angiogenesis, and vascularity1. Therefore, on the basis of conventional MRI, permeability and perfusion MRI sequences could provide additional important information on diagnosis, treatment response, and survival prediction. Currently, dynamic contrast-enhanced (DCE) MRI is widely used to quantify BBB permeability-related properties, such as transfer constant (Ktrans), fractional plasma volume (vp), and fractional extravascular-extracellular volume (ve), and dynamic susceptibility contrast MRI (DSC) is used to quantify perfusion-related properties, such as cerebral blood volume (CBV) and cerebral blood flow (CBF). We recently developed an MR multitasking-based dynamic imaging for cerebrovascular evaluation (MT-DICE) technique for simultaneous quantification of permeability and leakage-insensitive perfusion with single-dose contrast injection2. In this work, we conducted a clinical study to assess the real-world performance of MT-DICE in patients with brain tumors.Methods
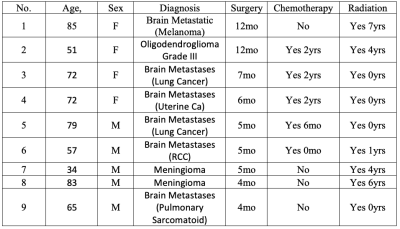
Study ParticipantsNine patients (aged 34–85 y, 4 females) with known brain tumors were recruited with informed consent, including one patient with oligodendroglioma (Grade III), two patients with meningioma, and six patients with brain metastases. All subjects had received radiation therapy (0.2-7 years).
Imaging Acquisition
All imaging experiments were performed on a 3T clinical MR scanner (MAGNETOM Vida; Siemens Healthcare, Erlangen, Germany) with a 20-channel head-neck coil. The MT-DICE sequence was incorporated into a clinical MR study and acquired without any preload contrast bolus. The clinical protocol included pre-contrast T2-FLAIR, pre-contrast T2, diffusion-weighted imaging, and pre- and post-contrast T1. MT-DICE imaging was performed in an oblique transverse orientation with the following imaging parameters: field-of-view (FOV) = 216 × 216 × 128 mm3, spatial resolution = 1.5 × 1.5 × 4.0 mm3, pulse repetition time = 19.30 ms, echo times = 2.46/4.92/7.38/9.84/12.30/17.22 ms, saturation recovery period (the temporal resolution of dynamic T1∕T2* mapping) is approximately 1.2 s, flip angle = 10◦, total time = 7.6 min. Single dose (0.1 mmol/kg of body weight) of gadobenate dimeglumine (MultiHance; Bracco Imaging, Milan, Italy) was administered through antecubital intravenous access 60 seconds into the scan at the rate of 3.0 mL/s, followed by a 20 mL saline flush at the same rate.
Image analysis
All images were analyzed independently by two readers who were blinded to the patients’ clinical information (8 years and 15 years of experience in neuroimaging, respectively). When multiple lesions were presented, the largest was selected for quantitative analysis. Two freehand regions of interest (ROIs) were drawn at the maximally enhanced region on post-contrast T1 and peritumoral hyperintense region on T2-FLAIR images, respectively, avoiding necrotic tissue and large vessels. Color-coded DCE (Ktrans, Vp, and Ve) and DSC (CBV and CBF) maps were generated. The same ROIs were then positioned on DCE and DSC maps. For DSC, an extra ROI was drawn in the contralateral normal-appearing white matter as references for normalization (rCBV and rCBF). The measurement results of the two readers were used to assess the interobserver reliability. The average of the two measurement results was used for further analysis.
Statistical Analysis
Inter-reader reliability of the parameters was assessed by the intraclass correlation coefficient (ICC). ICC values of ≤0.40, between 0.41 and 0.60, between 0.61 and 0.80, and ≥0.81 were interpreted as poor, moderate, good, and excellent reliability, respectively. The means or medians of the DCE and DSC parameter values measured from post-contrast T1 (i.e. intratumoral maximal enhanced region) and T2-FLAIR (peritumoral T2-hyperintense region) were compared using the Student’s t test or the Mann-Whitney U test.
Results
Of the 9 patients included in the study, 1 had progression and 8 were stable at 3-month clinical follow-up. Clinical characteristics including age, sex, and treatment are shown in Figure 1.The interobserver reliability was excellent for Ktrans in the peritumoral T2 hyperintense region (ICC = 0.82) and was good for Vp (ICC = 0.80) and Ve (ICC = 0.74). In the intratumoral maximal enhanced region, all the parameters demonstrated excellent reliability (ICC = 0.86-0.89).
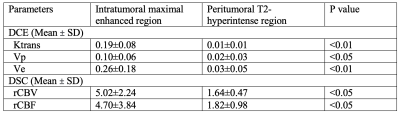
As shown in Figure 2, all the quantitative parameters from DCE and DSC were significantly higher in the contrast-enhanced area than in the peritumoral T2 hyperintense area (p < 0.01).
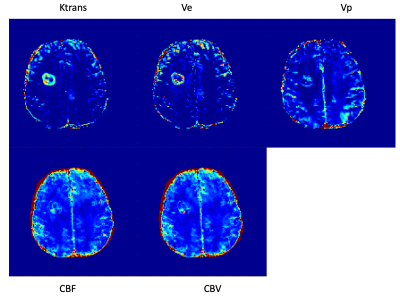
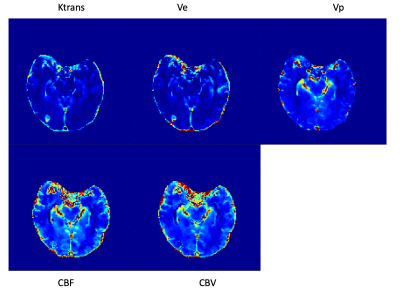
Figures 3 and 4 show examples of multiparametric MR images of a patient with brain metastases (lung cancer) and a patient with brain metastases (pulmonary sarcomatoid), respectively.
Discussion
Brain tumors represent a great therapeutic challenge. In this work, we incorporated the newly developed MT-DICE technique to achieve simultaneous DCE and DSC acquisition with a single-dose injection in clinical patients. As expected, the tumoral region showed worse BBB disruption and higher perfusion than the surrounding tissue, which suggested more severe condition.Acknowledgements
None.References
1. Carmen-Orozco RP, Dávila-Villacorta DG, Cauna Y, Bernal-Teran EG, Bitterfeld L, Sutherland GL, Chile N, Céliz RH, Ferrufino-Schmidt MC, Gavídia CM, Sterling CR, García HH, Gilman RH, Verástegui MR. Blood-brain barrier disruption and angiogenesis in a rat model for neurocysticercosis. J Neurosci Res. 2019 Feb;97(2):137-148. doi: 10.1002/jnr.24335. Epub 2018 Oct 13. PMID: 30315659; PMCID: PMC7011581.
2. Hu Z, Christodoulou AG, Wang N, Xie Y, Shiroishi MS, Yang W, Zada G, Chow FE, Margol AS, Tamrazi B, Chang EL, Li D, Fan Z. MR multitasking-based dynamic imaging for cerebrovascular evaluation (MT-DICE): Simultaneous quantification of permeability and leakage-insensitive perfusion by dynamic T1/T2* mapping. Magn Reson Med. 2023 Jan;89(1):161-176. doi: 10.1002/mrm.29431. Epub 2022 Sep 21. PMID: 36128892.
Figures