2293
Abnormalities of Grey Matter Volume in Parkinson’s Disease with Depression: A Voxel-Based Morphometry Study1Department of Radiology, the First Affiliated Hospital of Dalian Medical University, Dalian, China, 2GE Healthcare, Beijing, China
Synopsis
Keywords: Parkinson's Disease, Parkinson's Disease, Voxel-Based Morphometry、Parkinson's disease with depression
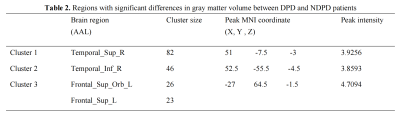
Depressive symptoms are common in Parkinson’s disease (PD), but the pathophysiology and neural basis underlying depression in PD is complex. To shed more light on the abnormal regions and distribution characteristics of gray matter in PD patients with depression (DPD), we conducted a Voxel-Based Morphometry (VBM) study. Compared with PD with non-depression (NDPD) patients, the gray matter volume of DPD patients decreased abnormally in the right superior temporal gyrus, right inferior temporal gyrus, left orbital superior frontal gyrus and left dorsolateral superior frontal gyrus. We speculate that changes in the brain regions are essential in the pathophysiology of DPD.Introduction
Parkinson's disease (PD) is a neurodegenerative disease that classically presents with resting tremors, bradykinesia, postural instability, and rigidity. Recently, the importance of mood disorders in PD has been recognized, as it affects the quality of life and disease progression in PD patients. The incidence of depression in PD patients is higher than in the general elderly or patients with other chronic or disabling diseases[1]. Basic research has confirmed that Lewy body accumulation in specific brain areas of PD patients may damage emotion-related functions, leading to depression[2]. VBM is based on voxel level analysis of brain MRI, through quantitative calculation of brain gray matter density and volume changes accurately show the morphological changes of brain tissue. This study used the VBM method to explore the whole brain gray matter volume change patterns of DPD patients and analyze the relationship between abnormal brain regions and DPD-related clinical symptoms.Materials and Methods
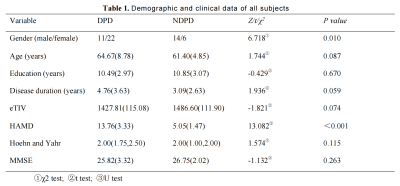
53 clinically confirmed PD patients were recruited, and all were right-handed. All patients with PD were divided into two groups according to their scores on the Hamilton Depression scale (HAMD): with a HAMD score of >7 in the DPD group (33 cases, 11 males, mean age: 64.67±8.78 years) and a HAMD score of ≤7 in the NDPD group (20 cases, 14 males, mean age: 61.4±4.85 years). Participants were scanned using a 3.0 T GE Signa HDXT scanner from America equipped with an 8-channel head coil. On whole-brain, 3D magnetization-prepared rapid-acquisition gradient-echo T1-weighted sequence was acquired: repetition time = 10.2 ms, echo time (shortest) = 4.2 ms, flip angle = 13°, FOV = 24 × 24cm2, matrix size = 256 × 256, voxel size = 1.0 × 1.0 × 1.0 mm, slice thickness 1.0 mm. The VBM was performed on the dataset as an alternative method of detecting atrophy in the whole brain gray matter, using MATLAB R2013b (Mathworks, Natick, MA) and SPM8 (Wellcome Department of Cognitive Neurology, London). Data analyses were performed using SPM8, independent-sample t-test was used to compare the whole brain gray matter volume between the DPD group and the NDPD group. Age, gender, education, and estimated total intracranial volume (eTIV) were included as covariates. P<0.05 (FDR corrected) and voxel threshold ≥ 20 were statistically significant.Results
No significant differences were observed between the two groups in age, education, Disease duration, eTIV, Hoehn and Yahr and MMSE score (P > 0.05). The HAMD score of the DPD group was significantly higher than that of the NDPD group (P < 0.001) (Table 1). Compared with the NDPD group, the gray matter volumes of the Temporal_Sup_R, Temporal_Inf_R, Frontal_Sup_Orb_L and Frontal_Sup_L were significantly reduced in the DPD group (Table 2, Figure 1).Discussion
VBM is an unbiased technique widely used to observe differences in the anatomical structure of living nerves. It is based on voxel-level analysis of brain MRI through quantitative calculation of brain local gray matter density and volume changes to show the morphological changes of brain tissue accurately. This study showed that compared with NDPD patients, the gray matter volume of right superior temporal gyrus (STG), right inferior temporal gyrus (ITG), left orbital superior frontal gyrus and left dorsolateral superior frontal gyrus reduced in DPD patients. The frontal-limbic system involves memory, emotional perception and regulation, motivation and planning, and social behavior. Abnormal changes in the orbital superior frontal gyrus may cause 5-HT, DA, NE and other neurotransmitter production and transmission disorders, resulting in non-motor symptoms such as depression. The atrophy of related brain regions in DPD patients is more obvious than that in NDPD patients[3], which may explain its more serious emotional disorders. The temporal lobe is related to memory function and is also involved in the regulation of emotional and mental activities. The decrease of gray matter volume in the right STG and ITG may lead to obvious memory loss and emotional regulation disorders. The frontal lobe is the key neural mechanism to support advanced intelligent activities such as planning, thinking and problem-solving, and it undertakes higher integration functions in cognition. It has been reported that the functional continuity of the left dorsolateral prefrontal cortex (dlPFC) and the right STG in DPD patients is reduced. Microstructural asymmetry of dlPFC is closely related to moderate depression and may be a potential biomarker of depression[4]. In this study, compared with the NDPD group, DPD patients showed atrophy of the gray matter in the left dorsolateral superior frontal gyrus, which may indicate the neuroanatomical causes of depression.Conclusion
DPD patients have specific gray matter volume atrophy in depression-related brain regions closely related to their clinical symptoms. VBM technology may become an important means to monitor the development of DPD.Acknowledgements
Thank you to all colleagues involved in this studyReferences
[1] MELE B, HOLROYD-LEDUC J, SMITH EE, et al. Detecting anxiety in individuals with Parkinson disease: A systematic review [J]. Neurology, 2018, 90(1): e39-e47
[2] Gibb WR, Lees AJ. The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson's disease. J Neurol Neurosurg Psychiatry. 1988 Jun;51(6):745-52. doi: 10.1136/jnnp.51.6.745.
[3] Xie GQ, Wu KH, Bi Q, et al. Research progress of multimodal MRI and radiomics in evaluation of Parkinson's disease with depression[J]. Chin J Magn Reson Imaging, 2022, 13(6): 135-138.
[4] LOU Y, HUANG P, LI D, et al. Altered brain network centrality in depressed Parkinson's disease patients [J]. Mov Disord, 2016, 30(13): 1777-1784.