2272
The value of zero echo time MR imaging for demonstrating bony change of sacroiliac joint in ankylosing spondylitis: a comparative study with CT
Ziwei Zhang1, Lingling Song1, Weixin He1, Qi Zeng1, Lisha Nie2, Xiaocheng Wei2, Jiawei Wang1, He Sui1, Zhaoshu Huang1, Xia Zhu1, Chen Liang1, and Yu Li1
1The Affiliated Hospital of Guizhou Medical University, GuiYang, China, 2GE Healthcare, MR Research China, BeiJing, China
1The Affiliated Hospital of Guizhou Medical University, GuiYang, China, 2GE Healthcare, MR Research China, BeiJing, China
Synopsis
Keywords: Skeletal, Skeletal
The current study aims to compare the detection ability of zero echo time(ZTE) MRI and CT in presenting bony change of sacroiliac joint in ankylosing spondylitis. It was concluded that the ankylosing spondylitis detection rate was comparable between ZTE MRI and CT, where the detection rate of bony erosions by ZTE MRI was higher than that by CT. Our observations indicated that in the future, the ZTE MRI may potentially replace the ionization-related CT method by providing a more comprehensive evaluation of sacroiliitis in ankylosing spondylitis patients.Main findings
We found that for ankylosing spondylitis patients, ZTE MRI had comparable diagnostic efficiency with CT for bony structures, and had better performance in detecting bony erosions.Introduction
Ankylosing Spondylitis (AS) is a chronic inflammatory disease characterized by sacroiliitis, which evolves into joint ankylosis as the disease progresses [1]. It is universally acknowledged that CT is a commonly-used method to evaluate the severity of sacroiliitis, however, the ionizing radiation originating from CT examination may impact patient's fertility. Due to the nature of extremely short T2, the bone signal cannot be directly acquired by conventional MRI sequences. However, the recently developed zero echo time(ZTE) MRI technology can detect the cortical bone signal and provide information on bony change without radiation[2]. The clinical value of ZTE MRI in presenting bone structures has been reported, thus we assumed that ZTE MRI might be beneficial for observing AS patients’ cortical changes in the sacroiliac joint. Hence the purpose of our study was to demonstrate the clinical applicability of ZTE MRI in bony change of the sacroiliac joint in ankylosing spondylitis.Material and methods
After institutional review board approval and written informed consent, thirty-five patients from January 2021 to November 2021 were enrolled in our study. Inclusion criteria were as follows: patients meeting the diagnostic criteria for AS established by Ankylosing Spondylitis International Society in 2009[3] and having no contraindications to MR examination. Exclusion criteria included a history of previous surgery, other infections and tumors in the low back, and serious damage to the heart, brain, and hematopoietic system. Moreover, subjects who did not undergo CT examination or had poor MR image quality with gross artifacts were also excluded. Finally, a total of 21 cases were included for analysis, including 13 males with a mean age of 27.51 ± 5.75 years and 8 females with a mean age of 29.38 ± 10.77 years. All patients underwent ZTE MRI on a 3.0T MR scanner(MR750W, GE Healthcare) equipped with a 48-channel body-phased array coil. The parameters of ZTE sequence were as follows: TR= 1065 ms, TE= 0 ms, FOV=24cm×24cm, bandwidth=31.25kHz, flip angle=1°, thickness=1.4mm, resolution=256mm×256mm, scanning time=2min31s. The CT scan was performed with below main parameters: tube voltage=120kV, tube current=380mA, layer thickness=4mm, and matrix was 512×512. After ZTE scan was done, original images were transferred to the workstation and were post-processed on 3D-slicer and Image J. Two experienced radiologists graded ZTE images referring to the 1984 New York standard[4] independently. The presence of bilateral grade II or higher sacroiliitis or unilateral grade III-IV sacroiliitis was defined as a positive detection of AS, otherwise was negative. Furthermore, the detection of various abnormal imaging findings, including bony erosions, subarticular osteosclerosis, subsurface bony cystic changes, and joint space narrowing or widening, were also investigated. The intra-group correlation coefficient (ICC) was used to assess the agreement between the two readers' gradings. The Fisher exact probability was used to analyze the AS detection rate. The chi-square test was used to analyze the abnormal imaging findings detection rate. P values less than 0.05 were treated as statistically significant.Results
ICC test demonstrated the two physicians had a good agreement(ICC=0.897) in diagnosing the grade of sacroiliitis based on ZTE MR images. In this study, 18 patients were detected by ZTE MRI and 17 patients by CT. The difference in AS detection rate between the two methods was not statistically significant (P value > 0.05). As for abnormal imaging findings detection rate between ZTE MRI and CT, the results showed that the detection rate of bony erosion by ZTE MRI was higher than that by CT examination, and the difference was statistically significant (P < 0.01), while the rest of three findings shared no difference with CT(Table.1). In addition, we observed that ZTE MRI provided more visualized manifestation in bony erosions (Figure.1) than CT, especially in grade II and III sacroiliitis(Figure.2).Discussion and Conclusion
In this study, we found that the difference between ZTE MRI and CT was not statistically significant in the AS detection rate, indicating that ZTE MRI can show similar diagnostic efficiency as CT for bony structures, which is consistent with some authors’ opinions [5]. In a recent study[6], Li Y et al found ZTE MRI showed superior diagnostic performance in the depiction of sacroiliac joints structural lesions such as bony erosions, compared with routine T1-weighted MRI and had reliability comparable to CT. In our study of AS patients, we found the detection rate of bony erosions by ZTE MRI was higher than that by CT. In conclusion, for AS patients, ZTE MRI had comparable diagnostic efficiency with CT for bony structures and had better performance in detecting bony erosion. ZTE MRI can be brought into routine clinical MRI protocols to improve performance in the evaluation of bony structural changes in patients with ankylosing spondylitis.Acknowledgements
No acknowledgment found.References
[1] Deodhar A et al. Clin Rheumatol, 2016, 35(7): 1769-76.
[2] Weiger M et al. Magn Reson Med, 2013,70(2):328-32.
[3] Rudwaleit M et al. Ann Rheum Dis, 2009,68(6):777-83.
[4] van der Linden S et al. Arthritis Rheum, 1984,27(4):361-8.
[5] Xu YH et al. J Chin Acad Radiol, 2020,3(2):108-114.
[6] Li Y et al. Eur Radiol, 2022,32(6):3963-3973.
Figures
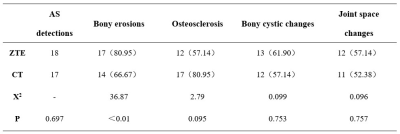
Comparison of (AS, abnormal
imaging findings) detection rate between ZTE MRI and CT.
A
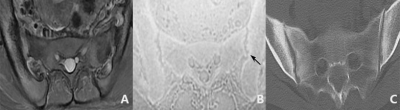
27-year-old female. (A) FST2 ax. Only blurring of the joint margins was seen. (B)ZTE image. Obvious
bony erosions were seen on image with the left
side more obvious(black arrow). (C) CT image. The bony erosions seen on CT
image were less clear.
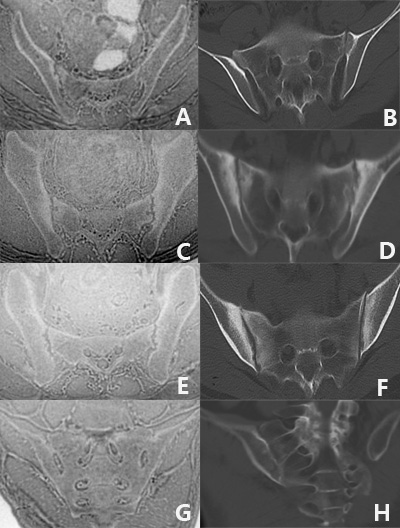
(A-B): A
22-year-old female, grade I. Subtle blurring of the joint margins was seen. (C-D): A 19-year-old male, grade II. Small localized
areas with erosions and sclerosis were seen. (E-F): A
27-year-old female, grade III. Obvious erosions and sclerosis were seen. (G-H): A 36-year-old male, grade IV. Complete ankylosing was seen.
DOI: https://doi.org/10.58530/2023/2272