2254
Attention-based Two Stage Deep Learning Model for the Segmentation and Classification of Pelvic and Sacral Tumors on Routine MRI1Department of Radiology, Peking University People's Hospital, Beijing, China
Synopsis
Keywords: MSK, Tumor
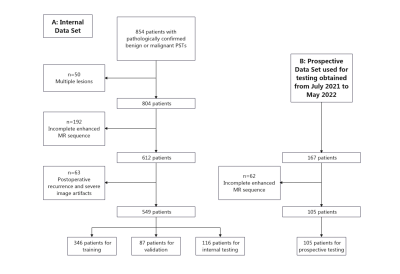
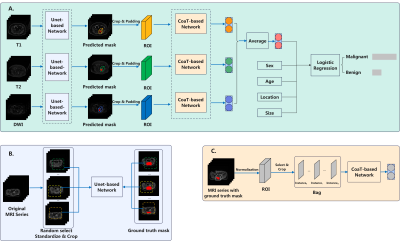
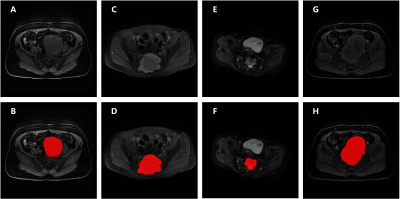
Early detection and correct diagnosis are key to adequate and successful treatment of PSTs. Based on multi-sequence MRI images, physician’s labeling, segmentation model, and clinical features, six classification models were built. The highest scoring model (model 6) achieved 0.836 AUC, 0.781 ACC in the prospective test set, which was comparable to that of senior residents and junior resident. However, the diagnosing time of DL model is significantly shorter than physicians. Our attention-based two stage DL model allowed the accurate segmentation and classification of benign and malignant PSTs without enhanced MRI and may thus facilitate diagnosis.Methods: 549 patients with benign or malignant PSTs at our hospital were retrospectively analyzed and used for model building and internal test. An additional 105 PSTs patients were used for prospective test set. Based on multi-sequence MRI images (T1-W, T2-W, DWI, CET1-W), physician’s labeling, segmentation model, and clinical features, we compared the effects of six classification models. Three radiologists compared diagnostic performance with the model. The performance of different models was assessed using the area under the curve (AUC), accuracy (ACC) values.
Results: In total, 654 patients were enrolled in this study, including 160 benign tumors and 494 malignant tumors. In this study, significant differences in sex, age, tumor size, and tumor location between benign and malignant PSTs were found (P < 0.01), consistent with the results of previous studies [2, 3]. For T1-w, T2-w, DWI and CET1-w sequences, Dice scores were 0.606, 0.792, 0.694, 0.728, and IoU values were 0.472, 0.678, 0.573 and 0.598, respectively. We found that the classification model based on segmentation outperformed the whole-map classification model and classification model based on the doctors’ rough segmentation annotation. The model based on plain MR images (without CET1-w) obtained an ACC comparable to that of the enhanced model (with CET1-w). The fusion of imaging and clinical information further improved the efficiency and robustness of the algorithm. Moreover, our highest scoring model (model 6) achieved mean Dice score of 0.758 for segmentations, 0.823 AUC, 0.802 ACC, 0.864 sensitivity, and 0.657 specificity for classifications in the internal test set, and 0.836 AUC, 0.781 ACC, 0.825 sensitivity, and 0.640 specificity in the prospective test set. The model’s ACC was comparable to that of senior residents (ACC of 0.819 and 0.771; P > 0.05) and junior resident (ACC of 0.79; P > 0.05). However, the diagnosing time of DL model (2.1 seconds) is significantly shorter than physicians (average time 4.32 minutes) (P < 0.01).
Conclusions: Our attention-based two stage DL model allowed the accurate segmentation and classification of benign and malignant PSTs without enhanced MRI and may thus facilitate diagnosis. Our model based on MR plain scan can helpful patients who are unwilling to undergo enhanced MR (e.g., children with fear of injections or person allergic to contrast media).
Acknowledgements
noReferences
[1]. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33.
[2]. Yin P, Zhi X, Sun C, Wang S, Liu X, Chen L, et al. Radiomics Models for the Preoperative Prediction of Pelvic and Sacral Tumor Types: A Single-Center Retrospective Study of 795 Cases. Front Oncol. 2021;11:709659.
[3]. Yin P, Mao N, Chen H, Sun C, Wang S, Liu X, et al. Machine and Deep Learning Based Radiomics Models for Preoperative Prediction of Benign and Malignant Sacral Tumors. Front Oncol 2020;10:564725.
[4]. Yin P, Mao N, Zhao C, Wu J, Chen L, Hong N. A Triple-Classification Radiomics Model for the Differentiation of Primary Chordoma, Giant Cell Tumor, and Metastatic Tumor of Sacrum Based on T2-Weighted and Contrast-Enhanced T1-Weighted MRI. J Magn Reson Imaging 2019;49(3):752-759.
[5]. Langevelde KV, Vucht NV, Tsukamoto S, Mavrogenis AF, Errani C. Radiological Assessment of Giant Cell Tumour of Bone in the Sacrum: From Diagnosis to Treatment Response Evaluation. Curr Med Imaging 2022;18(2):162-169.
Figures