2248
Predicion of Microvascular Invasion in Hepatocellular Carcinoma using Diffusion Kurtosis Imaging1The First Affiliated Hospital, Dalian Medical University, Dalian, China
Synopsis
Keywords: Liver, Blood vessels
Microvascular invasion (MVI) is an independent factor leading to poorer prognosis after liver resection and transplantation. In this retrospective study, we evaluated the discrimination power of Diffusion Kurtosis Imaging for predicting microvascular invasion Microvascular Invasion in hepatocellular carcinoma Hepatocellular Carcinoma (HCC). Our resuts showed that DKI-based quantitative parameters might have a certain value in identifying MVI status in HCC.Introduction
According to the latest statistics of global cancer estimates, hepatocellular carcinoma (HCC), as the most common hepatic malignancy, has ranked sixth with its incidence and third with its mortality among all cancers [1]. Microvascular invasion (MVI) is a definite factor leading to poorer prognosis after resection and liver transplantation. In the presence of MVI, tumor cells can spread and metastasize in the liver to form a portal vein tumor thrombus or multiple lesions or distant metastasis[2]. In clinical practice, MVI is diagnosed only by histopathological examination after operation, which limits its usefulness on clinical-decision making[3]. diffusion kurtosis imaging (DKI) can better describe the real diffusion process and probe the microstructure in biological tissues and displayed fascinating biomedical potential[4]. Therefore, it is important to predict MVI of HCC via a noninvasive way before surgery. In this study, we evaluate the performance of DKI parameters in predicting MVI of hepatic cancer (HCC).Materials and Methods
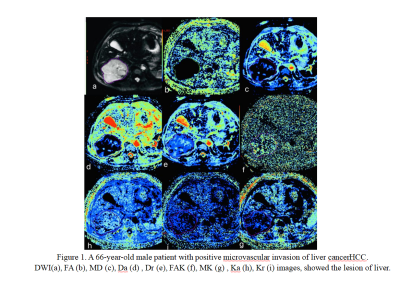
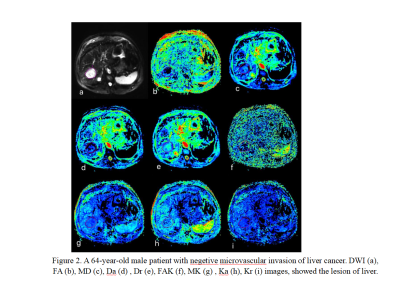
This study has been approved by the local IRB. A total of 63 cases with HCC in our hospital were retrospectively analyzed. The patients were divided into the MVI-positive group (n=22) and MVI-negative group (n=41). Routine MRI Ax T1 FSPGR, Ax T2 FSE, DWI sequence, Dual echo sequence, DKI sequence were acquired. Quantitative DKI-derived maps, including FA, MD, Da, Dr, FAK, MK, Ka, and Kr were automatically generated from DKI sequence by using the Functool software on GE AW 4.6 workstation. Referring to the lesion information obtained on DWI images, the FA, MD, Da, Dr, FAK, MK, Ka, and Kr maps were imported into the 3DSlicer-5.0.3 andAll images were analyzed by two abdominal radiologists (with 8 and 4 years of experience in abdominal imaging) who were blinded to the histopathological results. The whole tumor was incorporated into the volume of interest (VOI) in the DWI images of b800 using 3D slicer (version 5.0.3), an open source image processing software (www.slicer. org), with DWI images as the references. ROI Based on the lesion layer The area of the tumor should be as large as possible. The parameters of different DKI maps were calculated by the in-house prototyping software developed in 3DSlicer-5.0.3. The average values of each parameter map of all tumor sections were used for further statistical analysis. All data were analyzed using SPSS Ver.27.0 (SPSS Inc., Chicago, IL, USA). The significance of the inter-group difference of continuous data were determined using two-sided t-tests or the nonparametric Mann-Whitney U-test for normally or non-normally distributed data. Receiver operating characteristic (ROC) analysis was performed to evaluate diagnostic performance. A two-tailed P value less than 0.05 was considered to be statistically significant.Result
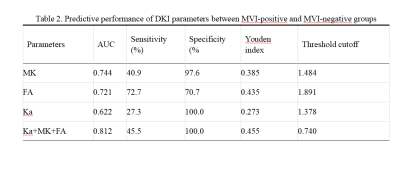
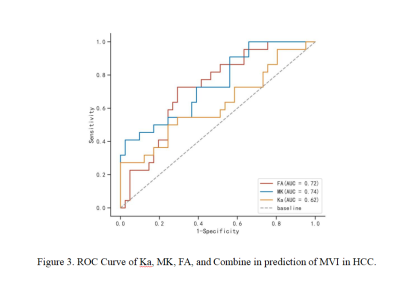
Table 1 shows the comparisons of parameters between MVI-positive and MVI-negative groups. The values of MK, Ka, and FA of MVI-negative group were significantly lower than those of the MVI-positive group (P < 0.05). Table 2 shows the AUC of MK, Ka, and FA for prediction of MVI were 0.744, 0.622, 0.721, and combination (Ka+MK+FA) were 0.812, respectively. When combination (Ka+MK+FA), the AUC was improved with a sensitivity of 45.5% and a specificity of 100% (cut-off value :0.740) .Discussion and Conclusion
According to the latest statistics, hepatocellular carcinoma (HCC) is the fifth most common cancer and the second most common cause of deaths in China[3]. LR and LT are currently the most important treatments[5]. Neverless, the recurrence rates of the treatments tend to be high[6]. Microvascular invasion (MVI) is a definite factor leading to poorer prognostic after resection and liver transplantation. In this study, MK value of the MVI-positive group was higher than that of the MVI -negative group, this maybe because that the presence of tumor emboli or tumor cell clusters in the portal vein, hepatic vein, or intravascular branch of the sac may limit the interaction of water molecules closest to the cell membrane in the extracellular heterogeneous medium in MVI-positive HCC. Ka value and FA value were higher in the MVI-positive group, which is consistent with the theory that higher kurtosis values indicate that water molecules disperse farther from the Gaussian distribution. This is consistent with the theory that larger kurtosis values indicate that the water molecule dispersion deviates from the Gaussian distribution, suggesting a more disturbed tissue structure. In conclusion, DKI parameters may be potential biomarkers for predicting MVI in HCC patients, which can provide surgeons with good prognostic information and better guide the choice of clinical surgery options.Acknowledgements
NoneReferences
[1] Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021;71(3):209–49.
[2]Lin Wang,Yue-Xinzi Jin,Ya-Zhou Ji,Yuan Mu,Shi-Chang Zhang,Shi-Yang Pan.Development and validation of a prediction model for microvascular invasion in hepatocellular carcinoma[J].World Journal of Gastroenterology,2020,26(14):1647-1659.
[3]Zhao Wei,Liu Wenguang,Liu Huaping,Yi Xiaoping,Hou Jiale,Pei Yigang,Liu Hui,Feng Deyun,Liu Liyu,Li Wenzheng. Preoperative prediction of microvascular invasion of hepatocellular carcinoma with IVIM diffusion-weighted MR imaging and Gd-EOB-DTPA-enhanced MR imaging.[J]. PloS one,2018,13(5).
[4] Tang L, Sui Y, Zhong Z, Damen FC, Li J, Shen L, et al. Non-Gaussian diffusion imaging with a fractional order calculus model to predict response of gastrointestinal stromal tumor to second-line sunitinib therapy. Magn Reson Med 2018;79(3):1399–406.
[5]Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020[J].Chinese Medical Journal English Edition,2021,134(07):783-791.
[6]Expert consensus on multidisciplinary diagnosis and treatment of precancerous lesions of hepatocellular carcinoma (2020 edition) [J]. J Clin Hepatol, 2020, 28(1): 14-20. DOI:10.3760/cma.j.issn.1007-3418. 2020.01.005.
Figures