2246
The value of IVIM for preoperative evaluation of liver regeneration after hepatectomy in hepatocellular carcinoma1Department of radiology, West China hospital, Sichuan Univeristy, Chengdu, China, 2MR Research China, GE Healthcare, Beijing,China, Beijing, China, 3Department of radiology, Sanya People’s Hospital, Sanya, China
Synopsis
Keywords: Liver, Diffusion/other diffusion imaging techniques, Liver regeneration; Intravoxel incoherent motion; Carcinoma, Hepatocellular; Hepatectomy
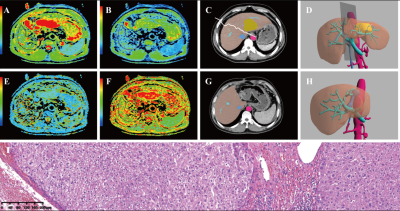
The D value derived from IVIM diffusion-weighted imaging may be a useful marker for the preoperative prediction of liver regeneration in patients with HCC. and the D value derived from IVIM diffusion-weighted imaging shows a significant negative correlation with fibrosis, an important predictor of liver regeneration. No IVIM parameters were associated with liver regeneration in patients who underwent major hepatectomy, but the D value was a significant predictor of liver regeneration in patients who underwent minor hepatectomy.Purpose
To evaluate the role of intravoxel incoherent motion (IVIM) parameters in the preoperative assessment of liver regeneration.Material and Methods
Fifty-four HCC patients (45 men and 9 women, mean age 51.26±10.41 years) were retrospectively analysed. The apparent diffusion coefficient (ADC), true diffusion coefficient (D), pseudodiffusion coefficient (D*), pseudodiffusion component fraction (f), diffusion distribution coefficient (DDC) and diffusion heterogeneity index (Alpha) were obtained by two independent radiologists. Spearman’s correlation test was used to assess correlations between IVIM parameters and the regeneration index (RI), calculated as 100% × (the volume of the postoperative remnant liver - the volume of the preoperative remnant liver) / the volume of the preoperative remnant liver. Multivariate linear regression analyses were used to identify the factors related to RI.Results
The intraclass correlation coefficient (ICC) ranged from 0.842-0.918. In all patients, the D value was a significant predictor (P<0.05) of RI in Spearman’s correlation test and multivariate analysis. The fibrosis stage was reclassified as F0–1 (n = 10), F2–3 (n = 26), and F4 (n = 18) using the METAVIR system. The D value showed a moderate correlation with fibrosis stage (r = -0.361, P=0.007). Furthermore, fibrosis stage showed a negative correlation with RI (r = -0.263, P=0.015). In the 29 patients who underwent minor hepatectomy, the D value showed a positive association (P<0.05) with RI in multivariate analysis and a negative correlation with fibrosis stage (r =-0.360, P=0.018). However, in the 25 patients who underwent major hepatectomy, no IVIM parameters were associated with RI (P>0.05).Conclusion
The D value may be a reliable preoperative predictor of liver regeneration.Acknowledgements
This work was supported by Science and Technology Support Program of Sichuan Province (Grant number 2021YFS0021、2021YFS0144), Post-Doctor Research Project, West China Hospital, Sichuan University (Grant number 2020HXBH130),References
1. Zhang T, Wei Y, He X et al (2021) Prediction of Remnant Liver Regeneration after Right Hepatectomy in Patients with Hepatocellular Carcinoma Using Preoperative CT Texture Analysis and Clinical Features. Contrast Media Mol Imaging 2021:5572470
2. Fruscione M, Pickens R, Baker EH et al (2019) Robotic-assisted versus laparoscopic major liver resection : analysis of outcomes from a single center. HPB (Oxford) 21:906-911
3. Kele PG, de Boer M, van der Jagt EJ et al. (2012) Early hepatic regeneration index and completeness of regeneration at 6 months after partial hepatectomy. Br J Surg 99:1113-1119
4. Pulitano C, Crawford M, Joseph D et al. (2014) Preoperative assessment of postoperative liver function: the importance of residual liver volume. J Surg Oncol 110:445-450
5. Haimerl M, Schlabeck M, Verloh N et al. (2016) Volume-assisted estimation of liver function based on Gd- EOB-DTPA-enhanced MR relaxometry. Eur Radiol 26:1125-1133 19. Park J, Kim JH, Kim JE et al. (2020) Prediction of liver regeneration in recipients after living-donor liver transplantation in using preoperative CT texture analysis and clinical features. Abdom Radiol (NY) 45:3763-3774 20. Park YS, Park SH, Lee SS, et al (2011) Biopsy-proven nonsteatotic liver in adults: estimation of reference range for difference in attenuation between the liver and the spleen at nonenhanced CT. Radiology 258:760-766 6. Bedossa P, Poynard T (1996) An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology 24:289-293 22. Scheuer PJ (1991) Classification of chronic viral hepatitis: a need for reassessment. J Hepatol 13:372-374
7. Le Bihan D, Ichikawa S, Motosugi U (2017) Diffusion and Intravoxel Incoherent Motion MR Imaging-based Virtual Elastography: A Hypothesis-generating Study in the Liver. Radiology 285:609-619 26. Le Bihan D, Breton E, Lallemand D, Aubin ML, Vignaud J, Laval-Jeantet M (1988) Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology 168:497-505
8. Bennett KM, Schmainda KM, Bennett RT, Rowe DB, Lu H, Hyde JS (2003) Characterization of continuously distributed cortical water diffusion rates with a stretched-exponential model. Magn Reson Med 50:727-734
9. Lai V, Lee VH, Lam KO, Sze HC, Chan Q, Khong PL (2015) Intravoxel water diffusion heterogeneity MR imaging of nasopharyngeal carcinoma using stretched exponential diffusion model. Eur Radiol 25:1708-1713
10. Seo N, Chung YE, Park YN, Kim E, Hwang J, Kim MJ (2018) Liver fibrosis: stretched exponential model outperforms mono-exponential and bi-exponential models of diffusion-weighted MRI. Eur Radiol 28:2812-2822
11. Slinker BK, Glantz SA (1985) Multiple regression for physiological data analysis: the problem of multicollinearity. Am J Physiol 249:R1-12.
12. Huebert RC, Shah VH (2014) Sinusoidal endothelial cells direct traffic at the intersection of regeneration and fibrosis. Hepatology 60:754-756
13. Wiemann SU, Satyanarayana A, Tsahuridu M et al (2002) Hepatocyte telomere shortening and senescence are general markers of human liver cirrhosis. FASEB J 16:935-942
14. Ding BS, Cao Z, Lis R et al (2014) Divergent angiocrine signals from vascular niche balance liver regeneration and fibrosis. Nature 505:97-102
15. Chow AM, Gao DS, Fan SJ et al (2012) Liver fibrosis: an intravoxel incoherent motion (IVIM) study. J Magn Reson Imaging 36:159-167
16. Moreno AH, Burchell AR, Rousselot LM, Panke WF, Slafsky F, Burke JH (1967) Portal blood flow in cirrhosis of the liver. J Clin Invest 46:436-445
17. Ren H, Liu Y, Lu J et al (2021) Evaluating the clinical value of MRI multi-model diffusion-weighted imaging on liver fibrosis in chronic hepatitis B patients. Abdom Radiol (NY) 46:1552-1561
18. Zipprich A, Steudel N, Behrmann C et al (2003) Functional significance of hepatic arterial flow reserve in patients with cirrhosis. Hepatology 37:385-392
19. Bai Y, Lin Y, Tian J et al (2016) Grading of Gliomas by Using Monoexponential, Biexponential, and Stretched Exponential Diffusion-weighted MR Imaging and Diffusion Kurtosis MR Imaging. Radiology 278:496-504
20. Park JH, Seo N, Chung YE et al (2021) Noninvasive evaluation of liver fibrosis: comparison of the stretched exponential diffusion-weighted model to other diffusion-weighted MRI models and transient elastography. Eur Radiol 31:4813-4823
21. Anderson SW, Barry B, Soto J et al (2014) Characterizing non-gaussian, high b-value diffusion in liver fibrosis: Stretched exponential and diffusional kurtosis modeling. J Magn Reson Imaging 39:827-834
22. Standish RA, Cholongitas E, Dhillon A, Burroughs AK, Dhillon AP (2006) An appraisal of the histopathological assessment of liver fibrosis. Gut 55:569-578
23. Biagini G, Ballardini G (1989) Liver fibrosis and extracellular matrix. J Hepatol 8:115-124
24. Sandrasegaran K, Territo P, Elkady RM, et al (2018) Does intravoxel incoherent motion reliably stage hepatic fibrosis, steatosis, and inflammation? Abdom Radiol (NY) 43:600-606
25. Manning P, Murphy P, Wang K, et al (2017) Liver histology and diffusion-weighted MRI in children with nonalcoholic fatty liver disease: A MAGNET study. J Magn Reson Imaging 46:1149-1158
26. Lefebvre T, Hébert M, Bilodeau L, et al (2021) Intravoxel incoherent motion diffusion-weighted MRI for the characterization of inflammation in chronic liver disease. Eur Radiol 31:1347-1358
27. Abdalla EK, Denys A, Chevalier P, Nemr RA, Vauthey JN (2004) Total and segmental liver volume variations: implications for liver surgery. Surgery 135:404-410
28. Kim JE, Kim JH, Park SJ, Choi SY, Yi NJ, Han JK (2019) Prediction of liver remnant regeneration after living donor liver transplantation using preoperative CT texture analysis. Abdom Radiol (NY) 44:1785-1794
29. Meier M, Andersen KJ, Knudsen AR, Nyengaard JR, Hamilton-Dutoit S, Mortensen FV (2016) Liver regeneration is dependent on the extent of hepatectomy. J Surg Res 205:76-84
30. Gruttadauria S, Parikh V, Pagano D et al (2012) Early regeneration of the remnant liver volume after right hepatectomy for living donation: a multiple regression analysis. Liver Transpl 18:907-913
31. Ma HY, Dong L, Quan SZ, Li RY, Wang XR (2021) Comparison of four markers of hepatic fibrosis and hepatic function indices in patients with liver cirrhosis and hepatoma. Ann Palliat Med 10:4108-4121
32. Cheemerla S, Balakrishnan M (2021) Global Epidemiology of Chronic Liver Disease. Clin Liver Dis (Hoboken) 17:365-370
33. Nadalin S, Testa G, Malagó M et al (2004) Volumetric and functional recovery of the liver after right hepatectomy for living donation. Liver Transpl 10:1024-1029
34. Yokoi H, Isaji S, Yamagiwa K et al (2005) Donor outcome and liver regeneration after right-lobe graft donation. Transpl Int 18:915-922
35. Gong WF, Zhong JH, Lu Z et al (2019) Evaluation of liver regeneration and post-hepatectomy liver failure after hemihepatectomy in patients with hepatocellular carcinoma. Biosci Rep 39
36. Haga J, Shimazu M, Wakabayashi G et al (2008) Liver regeneration in donors and adult recipients after living donor liver transplantation. Liver Transpl 14:1718-1724
Figures