2236
Preoperative prognostic Stratification for Patients with HCC Using Gadoxetic acid-enhanced MR Imaging1Radiology, West China Hospital, Chengdu, China, 2West China Hospital, Chengdu, China, 3MR Research China,GE Healthcare, Beijing, China, Beijing, China
Synopsis
Keywords: Liver, Cancer
Accurate preoperative risk stratification is of critical importance for determine patients who will benefit from liver resection. Our study developed three subgroups of patients with HCC associated with different prognosis (RFS and OS) after resection based on preoperative MR imaging features using the Survival Classification and Regression Tree (CART) method. The generated subgroups using CART method demonstrated good discriminatory for preoperatively stratification of the prognosis. Therefore, the CART model of this present study may help clinicians to consider non-surgical treatment more often in worse prognostic patients and as well as inform more intense surveillance following resection.Background and purpose
Hepatocellular carcinoma (HCC) is the sixth most common cancer and the third leading cause of cancer-related death worldwide in 2020(1). Although liver resection is feasible, safe, oncologically efficient and offers the best chance of a potential cure for resectable HCC, the prognosis of these patients is still discouraing, with a median overall survial ranging from 19.4 to 30 months(2). Indeed, 40% to 70% of patients with HCC will experience an early ecurrence (ER) following resection(2-4). The presence of ER is a bad feature that indicates inherent aggressive biological behaviors and heterogeneity of HCC and predicts worse prognosis.HCC tissue usually exhibits high molecular heterogeneity which is mainly documented at the intertumor (tumor by tumor) and intratumor (within each tumor) level(5). Currently, the molecular and immunological characterization of HCC is determined on histologic examination of the surgical specimens obtained after surgery(7-9). Therefore, the influence of the heterogeneity evaluationon on preoperative decision making is limited. An accurate preoperative estimation of patients who benefit most and least from resection and making precised risk stratifications before surgery is important to construct individualized therapeutic and survelliance strategies and improve the overall prognosis. As if liver resection is considered for patients who will not benefit following resection, an alternative treatment strategy for these patients, including adjuvant therapy or other nonsurgical treatment were recommended.Many efforts on preoperative prognostic strafifications and classification of HCC have been made in recent years. Some authors (6, 7) have reported that the radiological features based on gadoxetic acid–enhanced magnetic resonance (MR) imaging, such as peritumoral hypointensity on hepatobiliary phase (HBP), were independent risk factors of HCC. However, others stated that these studies need further validation to avoid potential observer bias. Due to the lack of a specific and practical predictive method, development of a predictive model that incorporates factors associated with risk stratifications based on preoperative clinic and imaging data is urgently warranted(10). Of all the available models, the survival classification and regression tree (CART) model, a useful unsupervised machine-learning statistical technique, has been used to identify homogeneous groups in health care to assist treatment decision making and improve predictive accuracy(8, 9). However, to our knowledge, no study has tried CART analysis relative to prognosis based on preoperative factors in HCC.The purpose of this study was to identify groups of patients with distinct outcomes and characterize HCC patients who derived the most or least benefit from surgery using CART model based on preoperative clinic and gadoxetic acid-enhanced imaging features.
Methods
This study was in accordance with the ethical guidelines of the Declaration of Helsinki, and was approved by the Institutional Review Board.180 patients from two institutions with gadoxetic acid-enhanced MR imaging between January 2015 and December 2018. All the MR examinations were performed by using 3.0-T MR scanner (Magnetom Skyra, Siemens Healthcare; MR 750, GE Healthcare). Three board-certified abdominal radiologists independently reviewed the MR images according to the LI-RADS v2018. The routine survelliant methods including CT, US and MRIwere used for the postoperative recurrence monitoring.The survival classification and regression tree method, was used to generate homogeneous groups of patients associated with OS based on the selected risk features. For subgroup analysis, multivariable Cox proportional hazard model using backward stepwise selection with Akaike information criterion (AIC) to assess risk factors .Results
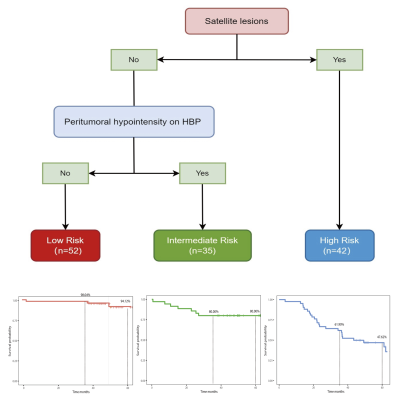
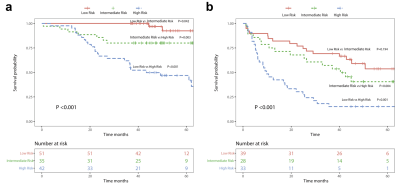
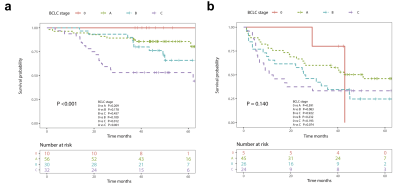
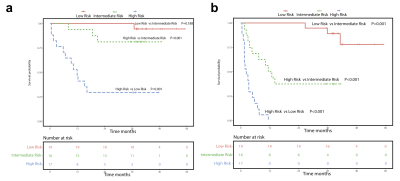
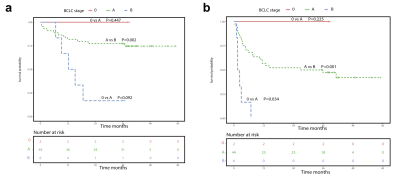
Three different prognostic groups including low risk (n=51) , intermediate risk (n=35) and high risk were finally generated by using CART model (Figure 1).In the training group, patients of low-, intermediate- and high risk group had an incremental worse 5-year OS (low risk, 94.12% vs. intermediate risk, 80.00% vs. high risk, 47.62%, P<0.001) (Figure 2a) and 3-year RFS (low risk, 69.23% vs. intermediate risk, 57.14% vs. high risk, 15.16%, P<0.001) (Figure 2b). Similarly, the 3-year OS among low-, intermediate- and high risk group were 98.04%, 80.00% and 61.90%, respectively. And the 1-year RFS among low-, intermediate- and high risk group were 84.62%, 75.00%, and 45.45%, respectively.The discrimination power of the CART model was very good in discriminating the three prognostic subgroups in the training cohort (C-index: 0.741, 95% CI: 0.581-0.902) and the 2000 resampling bootstrapping validation cohort (C-index: 0.733, 95% CI: 0.665-0.811). However, the discrimination pefromance between the BCLC subgroups showed no statistical significance in the RFS (P=0.140) (Figure 3). Compared to the BCLC stage, the CART model achieved better discrimination performance for OS (P<0.001) and RFS (P<0.001) stratification.Specifically, patients deemed high risk also has a worse 3-year OS (low risk, 29.41% vs intermediate risk, 78.57% vs. high risk, 97.47%, P<0.001, Figure 4a) and 6-month RFS (low risk, 17.65% vs. intermediate risk, 68.75% vs. high risk, 100%, P<0.001, Figure 4b) compared with patients who were either intermediate or low risk in external validation group. Additionally, poor to moderate separation of surviva curve for OS (Figure 5a) and RFS (Figure 5b) was also obtained among all patients in external validation group using BCLC stage.Conclusions
The CART model can preoperatively stratify patients with distinct prognostic outcomes. It therefore provide useful information for determining treatment strategy, that is, patients who are likely to experience poor survival should consider more therapeutic schemes before or after surgery rather than upfront surgery.Acknowledgements
This work was supported by National Natural Science Foundation of China (grant number 82202117), China Postdoctoral Science Foundation (Grant number 2021M692289), Science and Technology Support Program of Sichuan Province (Grant number 2021YFS0144), Post-Doctor Research Project, West China Hospital, Sichuan University (Grant number 2020HXBH130) .References
1. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: a cancer journal for clinicians. 2021; 71(3):209-49.
2. Llovet JM, Kelley RK, Villanueva A, et al. Hepatocellular carcinoma. Nature reviews Disease primers. 2021; 7(1):6.
3. Vilarinho S, Calvisi DF. New advances in precision medicine for hepatocellular carcinoma recurrence prediction and treatment. Hepatology (Baltimore, Md). 2014; 60(6):1812-4.
4. Budhu A, Forgues M, Ye QH, et al. Prediction of venous metastases, recurrence, and prognosis in hepatocellular carcinoma based on a unique immune response signature of the liver microenvironment. Cancer cell. 2006; 10(2):99-111.
5. Jiang K, Al-Diffhala S, Centeno BA. Primary Liver Cancers-Part 1: Histopathology, Differential Diagnoses, and Risk Stratification. Cancer control : journal of the Moffitt Cancer Center. 2018; 25(1):1073274817744625.
6. An C, Kim DW, Park YN, Chung YE, Rhee H, Kim MJ. Single Hepatocellular Carcinoma: Preoperative MR Imaging to Predict Early Recurrence after Curative Resection. Radiology. 2015; 276(2):433-43.
7. Ahn SJ, Kim JH, Park SJ, Kim ST, Han JK. Hepatocellular carcinoma: preoperative gadoxetic acid-enhanced MR imaging can predict early recurrence after curative resection using image features and texture analysis. Abdominal radiology (New York). 2019; 44(2):539-48.
8. Wiener M, Acland KM, Shaw HM, et al. Sentinel node positive melanoma patients: prediction and prognostic significance of nonsentinel node metastases and development of a survival tree model. Annals of surgical oncology. 2010; 17(8):1995-2005.
9. Tsilimigras DI, Mehta R, Moris D, et al. A Machine-Based Approach to Preoperatively Identify Patients with the Most and Least Benefit Associated with Resection for Intrahepatic Cholangiocarcinoma: An International Multi-institutional Analysis of 1146 Patients. Annals of surgical oncology. 2020; 27(4):1110-9.
10. De Carlis L, Di Sandro S, Centonze L, et al. Liver-allocation policies for patients affected by HCC in Europe. Current transplantation reports. 2016; 3(4):313-8.
Figures