2153
The Performance of 3D-UTE MRI in Children with Pneumonia: Comparison with Standard 3D T1-GRE and T2-FSE Sequences1Key Laboratory of Birth Defects and Related Diseases of Women and Children(Sichuan University), Ministry of Education,West China Second university Hospital, Sichuan University, Chengdu, China, 2Central Research Institute, United Imaging Healthcare, shanghai, shanghai, China
Synopsis
Keywords: Lung, Pediatric, pediatric pneumonia
As a promising MRI technique, ultrashort echo‑time (UTE) sequence has been widely used in the evaluation of pulmonary diseases, allowing for increased contrast-to-noise ratio and the comparable image quality with CT. Literature on the use of the UTE in pneumonia is broadly available in older children and adults, whereas the data in younger children group is limited. This study illustrated the ability of UTE lung imaging for assessing pneumonia patients under 3 years old and has good diagnostic utility in detecting the typical morphological findings of pediatric pneumonia.Introduction
Pediatric pneumonia is a major cause of childhood mortality in the world[1], especially with both higher prevalence and death rate in younger patients group. Imaging assessment plays an essential role for diagnosis and follow-up evaluation. Due to the huge inter-observer variability of interpretation of radiographs [2, 3] and the ionizing radiation exposure of CT[4], MRI is more appropriate for evaluating pulmonary diseases in pediatric patients with no risk of radiation hazard[5]. UTE technique has shown its promising value in diagnosis of pneumonia[6], but most researches focused on older children or adults. Nevertheless, to the best of our knowledge, the diagnostic relevance of UTE in younger children with pneumonia was still uncertain. The goal of this study was to evaluate the potential of UTE in detecting the typical morphological findings of pneumonia patients under 3 years old, in comparison with the conventional T1 Gradient-Echo (T1-GRE) and T2 Fast Spin-Echo (T2-FSE) sequences.Methods
Seventy-seven eligible children with pneumonia (from 1 day to 2 years and 11 months) were imaged at a 3T pediatric MR scanner (Alpha, United Imaging Healthcare, Shanghai, China) using 3D-UTE, 3D-T1 GRE and T2-FSE. Subjective analysis was evaluated by two experienced pediatric radiologists. Overall image quality of visualization of the lung including the the presence of artifacts and lung parenchyma were assessed. Visualization of 6 pathological findings in pediatric pneumonia were estimated, including patchy increased intensity, atelectasis/consolidation, nodule/mass, bulla/cyst, interstitial lung disease/pulmonary fibrosis, and pleural effusion/ thickening, based on a 5-point scale. Interrater agreement was assessed using intraclass correlation coefficients (ICCs). Differences among three sequences were evaluated by Wilcoxon signed-rank test.Results
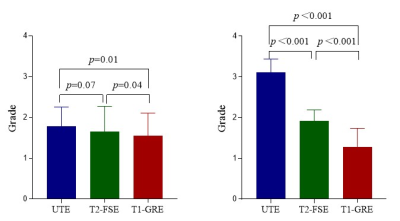
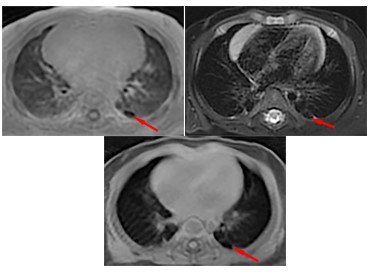
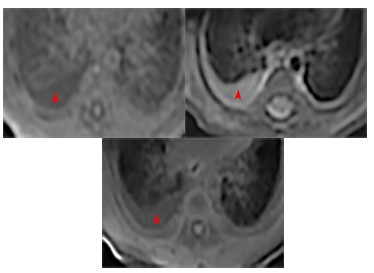
Inter-reader reliability for all evaluation were significant and determined as “excellent” or “substantial” (ICC = 0.75-1.00). The image artifacts of UTE were severer than T1-GRE (P=0.07) and equal to T2-FSE (P=0.07). visualization of lung parenchyma was significantly better for UTE than for T2-FSE (P<0.001) and T1-GRE (P<0.001). The visualization of the pathologies in most parameters (patchy increased intensity, atelectasis/consolidation, nodule/mass and bulla/cyst) was superior in UTE in comparison to T2-FSE and T1 GRE. Visualization scores of interstitial lung disease/pulmonary fibrosis between UTE and T2-FSE were similar and better than T1-GRE. On the case of pleural effusion/thickening, T2-FSE performed better than others. However, significant statistical differences between UTE with other sequences were only found in patchy increased intensity and atelectasis/consolidation.Discussion
This study illustrated the ability of UTE lung imaging for assessing pneumonia patients under 3 years old and has good diagnostic utility in detecting the typical morphological findings of pediatric pneumonia. Compared with T1-GRE and T2-FSE, the UTE sequence could yield superior image quality for the lung parenchyma and proved to be more reliable in the observation of patchy increased intensity, atelectasis/consolidation, nodule/mass, bulla/cyst, interstitial lung disease/pulmonary fibrosis. The interreader agreement was also slightly better in UTE, indicating a higher diagnostic certainty.Consolidation and patchy increased intensity always show higher proton density than adjacent natural lung parenchyma with poor signal intensity on MRI [2, 7]. The huge advantage of UTE in displaying lung parenchyma is bound to allow the significantly better visualization of pathological areas with increased proton density than spin echo and gradient echo, and UTE can be comparable to CT [8] , especially in the nodules[9, 10]. As to interstitial lung disease/pulmonary fibrosis, both UTE and T2-FSE yielded considerably superior results than T1-GRE, the promising performance of UTE was concordant with the results of Daniel Gräfe et al,[6] which could be ascribed to excellent inherent sensitivity of T2 and UTE for the high contrast provided by the liquid accumulation[5, 11] inside with interstitial tissue and fibrosis, and the better capability of displaying normal lung background. T2-FSE was superior than other two in the visualization of pleural effusion/ thickening, which is attribute to the considerable sensibility of FSE sequence to the high contrast provided by the liquid accumulation against the black background of normal parenchyma. The bulla/cyst was preeminently represented in UTE due to the absence of signal comparing to neighboring lung tissue. This indicates, that UTE MRI allows better evaluation of the pediatric pneumonia in younger children group.
The study has several limitations. First, it included a small number of study population recruited from a single center. Another limitation in this study could be the lack of lung CT image as standard of reference, whereas unnecessary CT examinations should be avoided in pediatric.
Conclusion
In conclusion, UTE MRI is a useful and potential method for evaluating pediatric pneumonia, which allowsproviding better or similar visualization of most pathological findings compared with T2-FSE and T1-GRE. We suggest that the UTE MRI techniques is well suited for pediatric population, especially in younger children with pneumonia thatwho requires longitudinal and repeated imaging for clinical care or research and is susceptible to ionizing radiation.Acknowledgements
NONEReferences
1. Scott JA, Brooks WA, Peiris JS, Holtzman D, Mulholland EK (2008) Pneumonia research to reduce childhood mortality in the developing world. J Clin Invest 118:1291-1300.https://doi.org/10.1172/jci33947
2. Yucel S, Aycicek T, Ceyhan Bilgici M, Dincer OS, Tomak L (2021) 3 Tesla MRI in diagnosis and follow up of children with pneumonia. Clin Imaging 79:213-218.https://doi.org/10.1016/j.clinimag.2021.05.027
3. Elemraid MA, Muller M, Spencer DA, Rushton SP, Gorton R, Thomas MF, Eastham KM, Hampton F, Gennery AR, Clark JE (2014) Accuracy of the interpretation of chest radiographs for the diagnosis of paediatric pneumonia. PLoS One 9:e106051.https://doi.org/10.1371/journal.pone.0106051
4. Liszewski MC, Görkem S, Sodhi KS, Lee EY (2017) Lung magnetic resonance imaging for pneumonia in children. Pediatr Radiol 47:1420-1430.https://doi.org/10.1007/s00247-017-3865-2
5. Sodhi KS, Ciet P, Vasanawala S, Biederer J (2022) Practical protocol for lung magnetic resonance imaging and common clinical indications. Pediatr Radiol 52:295-311.https://doi.org/10.1007/s00247-021-05090-z
6. Gräfe D, Anders R, Prenzel F, Sorge I, Roth C, Benkert T, Hirsch FW (2021) Pediatric MR lung imaging with 3D ultrashort-TE in free breathing: Are we past the conventional T2 sequence? Pediatr Pulmonol 56:3899-3907.https://doi.org/10.1002/ppul.25664
7. Hirsch FW, Sorge I, Vogel-Claussen J, Roth C, Gräfe D, Päts A, Voskrebenzev A, Anders RM (2020) The current status and further prospects for lung magnetic resonance imaging in pediatric radiology. Pediatr Radiol 50:734-749.https://doi.org/10.1007/s00247-019-04594-z
8. Ohno Y, Koyama H, Yoshikawa T, Seki S, Takenaka D, Yui M, Lu A, Miyazaki M, Sugimura K (2016) Pulmonary high-resolution ultrashort TE MR imaging: Comparison with thin-section standard- and low-dose computed tomography for the assessment of pulmonary parenchyma diseases. Journal of magnetic resonance imaging : JMRI 43:512-532.https://doi.org/10.1002/jmri.25008
9. Wielpütz MO, Lee HY, Koyama H, Yoshikawa T, Seki S, Kishida Y, Sakai Y, Kauczor HU, Sugimura K, Ohno Y (2018) Morphologic Characterization of Pulmonary Nodules With Ultrashort TE MRI at 3T. AJR American journal of roentgenology 210:1216-1225.https://doi.org/10.2214/ajr.17.18961
10. Ohno Y, Koyama H, Yoshikawa T, Kishida Y, Seki S, Takenaka D, Yui M, Miyazaki M, Sugimura K (2017) Standard-, Reduced-, and No-Dose Thin-Section Radiologic Examinations: Comparison of Capability for Nodule Detection and Nodule Type Assessment in Patients Suspected of Having Pulmonary Nodules. Radiology 284:562-573.https://doi.org/10.1148/radiol.2017161037
11. Geiger J, Zeimpekis KG, Jung A, Moeller A, Kellenberger CJ (2021) Clinical application of ultrashort echo-time MRI for lung pathologies in children. Clin Radiol 76:708.e709-708.e717.https://doi.org/10.1016/j.crad.2021.05.015
Figures