2144
Association of physical activity and screen time with DXA- and MRI-based body composition in adolescents, a population-based study1Department of Radiology and Nuclear Medicine, Erasmus MC, Rotterdam, Netherlands, 2Department of Public Health, Erasmus MC, Rotterdam, Netherlands, 3Department of Epidemiology, Erasmus MC, Rotterdam, Netherlands, 4Department of Pediatrics, Erasmus MC, Rotterdam, Netherlands
Synopsis
Keywords: Adolescents, Body, Body composition
This study is embedded in the Generation R Study, a population-based prospective cohort study in the Netherlands. At 13 years, whole-body Dixon MRI was performed. A previously presented Competitive Dense Fully Convolutional Network (CDFNet) was retrained and used to quantify the abdominal subcutaneous and visceral fat. We found a higher physical activity and lower screen time are associated with lower levels of MRI-based abdominal visceral obesity in adolescents. Therefore, promoting physical activity and reducing screen time should be one of the goals of lifestyle intervention programs for tackling the childhood obesity.INTRODUCTION
Childhood overweight and obesity have increased rapidly worldwide in last few decades, and they have harmful consequences in psychological and physical health that persist into adulthood 1. The promotion of more physical activity and less screen time has grown in response to this problem 2. It is widely recognized as a necessity in the context of a healthy lifestyle. Due to the impact of obesity persisting from early childhood to adolescence, a better understanding of the associations of physical activity and inactivity with obesity is needed 3. Prior studies have reported inconsistent associations of physical activity or screen time with overweight and obesity in children, and the majority of studies assessed body mass index (BMI) rather than body fat distribution 4,5. There is evidence demonstrating that the accumulation of abdominal subcutaneous fat and abdominal visceral fat can lead to insulin resistance, type 2 diabetes, and cardiovascular diseases in both adults and children 6. Therefore, the aim of the current study was to examine the associations of physical activity and screen time with body composition measures estimated by BMI, DXA and MRI in adolescents.METHODS
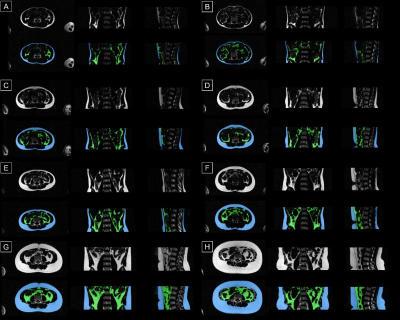
A total of 3,258 children aged 13 years from the Generation R Study, a population-based cohort study, were studied cross-sectionally (Figure 1). Measures of abdominal subcutaneous fat mass and abdominal visceral fat mass were obtained from whole-body Dixon MRI scans. A deep learning-based image segmentation method, using a 2D-Competitive Dense Fully Convolutional Network (CDFNet) as proposed in the FatSegNet method 7, was applied to extract the volumes of abdominal subcutaneous fat and visceral fat automatically (Figure 2). In addition, BMI and DXA-based measures (i.e., fat mass index (FMI), lean body mass index (LBMI) and android/gynoid fat mass ratio (A/G ratio)) were obtained. Physical activity and screen time were assessed via self-report questionnaires.RESULTS
A higher physical activity level was associated with a lower MRI-based abdominal visceral fat index (Z-score difference (95% CI): -0.11 (-0.20, -0.02)), a lower FMI and A/G ratio (-0.08 (-0.14, -0.01), -0.10 (-0.18, -0.03)), and higher LBMI (0.15 (0.08, 0.22)). A higher screen time was associated with a higher MRI-based abdominal subcutaneous fat index (0.03 (0.02, 0.05)) and visceral fat index (0.03 (0.01, 0.05)), BMI (0.02 (0.01, 0.04)), FMI (0.02 (0.01, 0.03) and A/G ratio (0.03 (0.02, 0.04)), and a lower abdominal visceral/subcutaneous fat mass ratio (V/S ratio) (-0.02 (-0.04, -0.01)) (Figure 3).DISCUSSION
Current findings highlight the importance of having adequate physical activity time in order to reduce the specific depots of abdominal fat in adolescents. To test our hypothesis, we used not only BMI and DXA, but also MRI to assess the comprehensive body composition measures, including abdominal subcutaneous fat and visceral fat. In line with our expectations, a higher physical activity time was associated with a reduction in total body fat and abdominal visceral fat, as we as an increase in total lean body mass. It was also expected that a higher physical activity time might be related to a lower abdominal subcutaneous fat, since physical activity was associated with total fat mass, and a strong correlation existed between total body fat and abdominal subcutaneous fat 8. However, no significance with regard to this association was found. In our study, we found significant associations of screen time with BMI and FMI but not with LBMI. Also, the associations between screen time and body composition measures including BMI, FMI, A/G ratio, abdominal subcutaneous fat index, abdominal visceral fat index and V/S ratio were a bit stronger compared to the associations of physical activity with these body composition measures. In fact, 2908 (93.1%) of children spent more than two hours per day on screen watching, which exceeds the recommendation from the American Academy of Pediatrics. At the same time, only 895 (29.2%) of children were compliant with current WHO guidelines on daily physical activity. This phenomenon might motivate future efforts in obesity prevention to reduce screen time and increase physical activity in children entering puberty.CONCLUSION
In adolescents, higher physical activity and lower screen time are linked to lower levels of MRI-based visceral adiposity. This information may be used to develop targeted intervention and prevention strategies that promote healthy behavior among adolescents.Acknowledgements
The Generation R study is managed by the Erasmus Medical Centre in close collaboration with the School of Law and the Faculty of Social Sciences at the Erasmus University, Rotterdam, the Municipal Health Service, Rotterdam area, and the Stichting Trombosedienst and Artsenlaboratorium Rijnmond (Star-MDC), Rotterdam. We gratefully acknowledge the contribution of children and their parents, general practitioners, hospitals, midwives and pharmacies in Rotterdam.
References
1. Alqahtani N, Scott J, Ullah S. Physical activity and sedentary behaviors as risk factors of obesity among rural adolescents. Journal of Child and Adolescent Behaviour. 2015.
2. Wilks DC, Besson H, Lindroos AK, Ekelund U. Objectively measured physical activity and obesity prevention in children, adolescents and adults: a systematic review of prospective studies. Obesity reviews. 2011;12(5):e119-e129.
3. Nader PR, O'Brien M, Houts R, et al. Identifying risk for obesity in early childhood. Pediatrics. 2006;118(3):e594-e601.
4. Ramires VV, Dumith SC, Gonçalves H. Longitudinal association between physical activity and body fat during adolescence: A systematic review. Journal of Physical Activity and Health. 2015;12(9):1344-1358.
5. Tripathi M, Mishra SK. Screen time and adiposity among children and adolescents: a systematic review. Journal of Public Health. 2020;28(3):227-244.
6. Gaggini M, Saponaro C, Gastaldelli A. Not all fats are created equal: adipose vs. ectopic fat, implication in cardiometabolic diseases. Hormone molecular biology and clinical investigation. 2015;22(1):7-18.
7. Estrada S, Lu R, Conjeti S, et al. FatSegNet: A fully automated deep learning pipeline for adipose tissue segmentation on abdominal dixon MRI. Magnetic resonance in medicine. 2020;83(4):1471-1483.
8. Tran TT, Yamamoto Y, Gesta S, Kahn CR. Beneficial effects of subcutaneous fat transplantation on metabolism. Cell metabolism. 2008;7(5):410-420.
Figures