2143
High resolution, swap free, and motion compensated water/fat separation in free-breathing pediatric T1-weighted abdominal MRI1Boston Children's Hospital, Harvard Medical School, Boston, MA, United States
Synopsis
Keywords: Liver, Pediatric, Abdominal MRI
T1-weighted GRE sequence with Dixon technique for water/fat separation is a routine component of abdominal MRI to detect lesions and characterize hemorrhage/fat content. The limitations of the routine free-breathing T1-weighted pediatric abdominal MRI and water/fat separation includes low-resolution to achieve high pixel-bandwidth and minimize chemical shift, respiratory motion blurring (despite radial acquisition) that degrades image sharpness, water/fat swapping, and off-resonance fat blurring due to multi-peak nature of fat spectrum. We have assessed a novel image acquisition and reconstruction pipeline based on 3-point Dixon method, multi-peak fat model, and residual motion correction to address all the limitations of the current practice.Purpose
The goal of this study was to evaluate water/fat separation using a high-resolution 3-point Dixon Golden angle radial acquisition with retrospective motion compensation and multi-peak fat modelling in in children undergoing abdominal MRI.Introduction
Water/fat separation in abdominal MRI in children plays an important role in monitoring and diagnosis of several pathological conditions such as hepatobiliary and kidney tumors and lesions. Unenhanced T1-weighted GRE acquisition is a routine component of pediatric abdominal MRI. To mitigate severe breathing motion artifacts in pediatrics with limited breath-hold capabilities (e.g., sedated patients), Volumetric Interpolated Breath-hold Examination (VIBE) with radial k-space sampling is utilized1. To minimize the chemical shift artifact high pixel bandwidth is required which does not allow for sufficient in-plane resolution to visualize fine details specially in small patients. In addition, although radial acquisition is less susceptible to motion, the residual motion-induced blurring is present in the images.Unlike water which has a single spectral peak, a single-peak fat model only accounts for 70% of the total fat protons resulting in off-resonance fat blurring thus application of multi-peak fat modelling is highly recommended for accurate water/fat separation2,3. Due to sensitivity of the 2-point Dixon technique to B0 field inhomogeneity, water/fat swapping artifact is sometimes present in the water/fat images which can be potentially mitigated by 3-point Dixon method4. The goal of this study was to evaluate the image quality using high-resolution 3-point Dixon acquisition with motion compensation and multi-peak fat modelling in children undergoing abdominal MRI.Methods
After obtaining consent, a high resolution (0.8x0.8x3mm3) T1-weighted 3-point Dixon (TEs = 1.45, 3.01, 4.6ms; TR = 4.61ms) radial-VIBE sequence with Golden Angle trajectory (TA=4’:20”) was acquired in thirteen pediatric (sedated) patients (4.3 ± 2.5 years old). This sequence was added to our routine abdominal MRI protocol which includes multi-plane fat-saturated T2-weighted sequences (BLADE), Diffusion-weighted imaging (DWI) and T1-weighted 2-point Dixon radial-VIBE (1x1x3mm3) (TA=3’:30”). All patients were scanned on a 3T MR scanner (MAGNETOM-Prisma, Siemens Healthineers, Germany) using a 30-channel body coil. Fat, water, and B0 field map were calculated from k-space data by iteratively solving the following optimization problem with the k-space-based data fidelity term that minimizes the difference between the measured k-space data ($$$y$$$) and the synthesized k-space based on the estimated water, fat, and field map ($$$W, F, ΔB_{0}$$$)5:$$W^*,F^*,∆B_0^*=argmin_{W,F,∆B_0}\sum_{coil,TE}‖K(W,F,∆B_0 )-y_{coil,TE}‖_2^2 $$Parallel imaging was applied through multiplying coil sensitivity maps ($$$coil_{s}$$$) by the estimated water and fat images in the data fidelity term.The k-space data ($$$K$$$) can be synthesized by calculating the contribution from single peak water spins ($$$W$$$), multi-peak fat spins ($$$F$$$) and the effect of the static field ($$$ΔB_{0}$$$) inhomogeneities as follows:$$K(W,F,∆B_0 )_{coil,TE}=FT(coil_{s}*exp(2πi*∆B_0*TE_n)*W)+D(TE_n )*FT(coil_s*exp(2πi*∆B_0*TE_n)*F) $$$$$D(TE_n )$$$ is the dephasing factor of fat relative to water that is used to model chemical shift in k-space. It accounts for the off-resonance fat blurring due to radial readout as follows5:$$D(TE_n )=\sum_{m=1}^m A_m*exp(2πi*∆f_m*TE_n)$$Where $$$m$$$ is the number of fat peaks considered in the model (i.e., 6), $$$A_m$$$ is the relative amplitude of each fat peak (adds up to one for all fat peaks), and $$$∆f_m$$$ is the resonance frequency offset of each peak with respect to water (ranging from 0.6 to 3.8 ppm).Residual respiratory motion was corrected through a soft-gating approach. The respiratory motion was calculated from the first echo by performing a Fourier transform along the z-direction of each projection angle followed by Principal Component Analysis (PCA). A weighting vector ([0,1]) was calculated based on the estimated respiratory motion and was applied to each projection6.The image reconstruction was performed in MatLab (The MathWorks, Natick, MA). The reconstructed images were assessed qualitatively in terms of presence of water/fat swapping and off-resonance fat blurring. To assess the effect of motion compensation and image sharpness the pre- and post-correction water and fat images were convolved with a 3x3 Laplacian kernel, and the variance of the response was calculated (Variance of Laplacian, VoL)7. A larger VoL represents a sharper (less blurry) image. In addition, an experienced radiologist reviewed the images and compared them to the clinical 2-point Dixon radial-VIBE images.Results
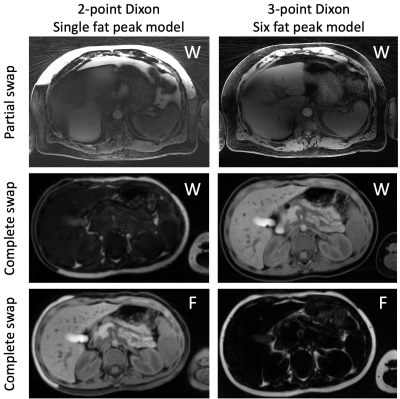
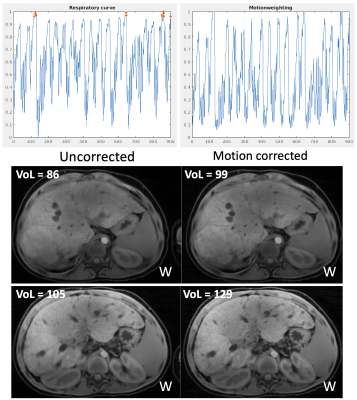
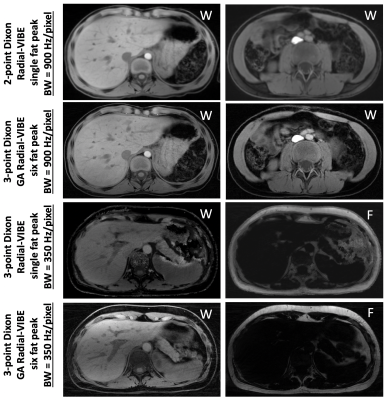
Water/fat swapping was observed in 9 out of 13 patients (69%) using the conventional 2-point Dixon technique while implementing the 3-point Dixon method with 6-peak fat model, eliminated the water/fat swapping artifact. Figure 1 shows two examples of the observed water/fat swapping artifact and the corresponding reconstructed images using the proposed pipeline. The variance of Laplacian (reflecting images sharpness) was significantly improved after residual motion correction (130 ± 32 vs. 104 ± 22). Two representative water images before and after motion correction along with the estimated respiratory motion curve are demonstrated in Figure 2. As shown in Figure 3 off-resonance fat blurring particularly with low bandwidth acquisition was significantly improved using the proposed acquisition/reconstruction approach. The radiologist rated all images (in-phase, out-of-phase, water, and fat) acquired and reconstructed using the proposed method superior to those reconstructed from the 2-point Dixon acquisition.Conclusion
High resolution Golden Angle radial-VIBE 3-point Dixon acquisition with 6-peak fat model and soft-gated motion correction eliminates water/fat swapping artifact, residual motion blurring and off-resonance fat blurring at the expense of ~1-minute additional acquisition time thus has great potential to replace the conventional T1-weighted 2-point Dixon, single fat peak technique.Acknowledgements
No acknowledgement found.References
1. Duffy, P. B. et al. Free-breathing radial stack-of-stars three-dimensional Dixon gradient echo sequence in abdominal magnetic resonance imaging in sedated pediatric patients. Pediatr Radiol 51, 1645–1653 (2021).
2. Hamilton, G. et al. In vivo characterization of the liver fat 1H MR spectrum. NMR Biomed 24, 784–790 (2011).
3. Wang, X., Hernando, D. & Reeder, S. B. Sensitivity of Chemical Shift-Encoded Fat Quantification to Calibration of Fat MR Spectrum. Magn Reson Med 75, 845 (2016).
4. Glover, G. H. & Schneider, E. Three-point Dixon technique for true water/fat decomposition with B0 inhomogeneity correction. Magn Reson Med 18, 371–383 (1991).
5. Benkert, T., Feng, L., Sodickson, D. K., Chandarana, H. & Block, K. T. Free-breathing volumetric fat/water separation by combining radial sampling, compressed sensing, and parallel imaging. Magn Reson Med 78, 565–576 (2017).
6. Zhang, T. et al. Fast pediatric 3D free-breathing abdominal dynamic contrast enhanced MRI with high spatiotemporal resolution. J Magn Reson Imaging 41, 460–473 (2015).
7. J. L. Pech-Pacheco, G. Cristobal, J. Chamorro-Martinez and J. Fernandez-Valdivia, "Diatom autofocusing in brightfield microscopy: a comparative study," Proceedings 15th International Conference on Pattern Recognition. ICPR-2000 3, 314-317 (2000)
Figures