2139
Feasibility of Blood oxygen level dependent magnetic resonance imaging for distinguishing HSPN from HSP in children Synopsis1The First Affiliated Hospital of Henan University of CM, Zhengzhou, China, 2Philips healthcare, Beijing, China
Synopsis
Keywords: Adolescents, Kidney
Blood oxygen level dependent magnetic resonance imaging (BOLD-MRI) could be used to detect renal tissue oxygen levels noninvasively, and the T2* time induced by the paramagnetic effect of deoxyhemoglobin can be obtained to indirectly assess blood oxygen utilization. Previous research has proven that BOLD-MRI can detect renal oxygenation levels with high sensitivity and the accuracy of the data has been validated by invasive probe measuring techniques. In this work, we investigated the clinical feasibility of T2* mapping for the detection of HSPN and HSP in children, since we predicted that HSPN would also result in aberrant renal blood oxygenation signals.
Summary of Principal Results
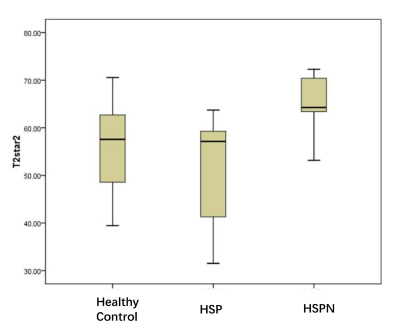
BOLD-MRI was demonstrated to be beneficial in the noninvasive evaluation of renal damage in children with HSPN. Renal cortical T2* levels were considerably greater in the HSPN group than in the HSP group (P < 0.05); Furthmore, its diagnostic efficiency in identifying HSPN and distinguishing it from HSP was higher.Introduction
BOLD-MRI is a noninvasive, radiation-free, and contrast-free method that can provide pictures with great spatial and temporal resolution. The inhomogeneous T2 relaxation time (T2*) produced from BOLD-MRI may aid in comprehending the oxygen content and metabolism of tissues, and thus represent the pathophysiological state of the kidney and dynamically evaluate the renal function and disease development. In numerous kidney disorders, including diabetic kidneys[5], lupus nephritis[6], and nephrotic syndrome[7], the feasibility of BOLD-MRI in measuring oxygenation status has been investigated. To our knowledge, however, few investigations on purpura nephritis have been published. Determining the clinical viability of BOLD-MRI in measuring the oxygenation state of HSPN and HSP and differentiating between HSPN and HSP was the objective of this investigation.Methods
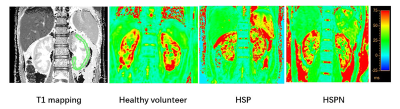
This research recruited 9 children with HSPN, 8 children with HSP, and 8 healthy volunteers (controls). On a 3.0T MR scanner (Ingenia CX, Philips HealthCare, The Netherlands), BOLD-MRI was peformed using standard renal transverse and coronal T2W MVXD imaging, followed by bilateral coronal renal B0 maps, breath-hold bilateral renal T1 mapping, and breath-hold bilateral T2* mapping scans. On the T1 map, the left renal cortical region of interest (ROI) was carefully drawn to prevent B0 inhomogeneity and the presence of visible artifacts. The ROI was transferred to the T1 and T2* maps, and the T1 and T2* values of the cortex were respectively retrieved. The normality and chi-square test of the grouped data was performed using the Kolmogorov-Smirnov and Levene's methods, and the measurements that fitted the normal distribution were represented by the mean ± standard deviation. A t-test on independent samples was performed to assess the differences between groups, with P < 0.05 indicating statistical significance. Using Spearman correlation analysis, potential relationships between clinical and MRI indicators were analyzed. Using ROC analysis, diagnostic performance and threshold values of the indices were determined.Results
In the HSPN group, T2* values were substantially higher than in the HSP group (P < 0.05). The AUC distribution of T2* for recognizing HSP and HSPN was 0.896%, with a threshold value of 63.74 ms and a specificity of 100%.Discussion
In this research, T2* values were considerably greater in the HSPN group than in the HSP group (P < 0.05), suggesting that the kidneys of children with HSPN maintain a certain level of high oxygen partial pressure. The findings were consistent with earlier research[8]. The acute phase of HSPN is brought on by decreased oxygen consumption in lost glomeruli and downstream tubules, as well as an increase in oxygen supply to the remaining glomeruli. This suggests that T2* values may serve as an MRI index for determining the severity of renal injury in HSPN and warrant further investigation.Conclusion
This research indicated that BOLD-MRI is beneficial for non-invasive evaluation of renal damage in children with HSPN, and renal cortical T2* values may be a relevant metric for differentiating between HSPN and HSP kidneys.Acknowledgements
No acknowledgement found.References
1.Li C, Liu H, Li X, et al. Application of BOLD-MRI in the classification of renal function in chronic kidney disease. Abdom Radiol (NY). 2019 Feb;44(2):604-611.
2.Thacker JM, Li LP, Li W, et al. Renal blood oxygenation level-dependent magnetic resonance imaging: a sensitive and objective analysis. Invest Radiol. 2015 Dec;50(12):821-7
3.Liang P, Chen Y, Li S, et al. Noninvasive assessment of kidney dysfunction in children by using blood oxygenation level-dependent MRI and intravoxel incoherent motion diffusion-weighted imaging. Insights Imaging,2021 Oct 21;12(1):146
4.Zhang JL, Morrel G, Rusinek H, et al. Measurement of renal tissue oxygenation with blood oxygen level-dependent MRI and oxygen transit modeling. Am J Physiol Renal Physiol.2014,306(6)::F579-87
5.Wang Q, Guo C, Zhang L, et al. BOLD MRI to evaluate early development of renal injury in a rat model of diabetes.J Int Med Res. 2018 Apr;46(4):1391-1403.
6.Zheng ZF, Wang YY, Yan TK, et al. Detection of renal hypoxia configuration in patients with lupus nephritis: a primary study using blood oxygen level-dependent MR imaging.Abdom Radiol (NY). 2021 May;46(5):2032-2044
7.Zhang R, Wang Y, Chen F, et al. Noninvasive evaluation of renal oxygenation in primary nephrotic syndrome with blood oxygen level dependent magnetic resonance imaging: Initial experience.J Int Med Res. 2015 Jun;43(3):356-63
8.Nishino T, Takahashi K, Ono S, et al. Fluctuation of R2* values in blood oxygenation level-dependent MRI during acute and remission phases of IgA vasculitis with nephritis in children. Jpn J Radiol. 2022 Aug;40(8):840-846