2127
Automated Fiber Quantification Predicts Motor Weakness in Patients Following Resection of Primary and Metastatic Brain Lesions
George Russell Glenn1, Sneha Sai Venkata Ka Mannam2, Chibueze Nwagwu3, Subir Goyal4, Gustavo Pradilla2, Edjah Kweku-Ebura Nduom2, Jeffery James Olson 2, David Painton Bray 2, and Hoang Bojanowski Kimberly2
1Diagnostic Radiology, Emory University, Lilburn, GA, United States, 2Neurosurgery, Emory University, Atlanta, GA, United States, 3College of Medicine, Emory University, Atlanta, GA, United States, 4Biostatistics and Bioinformatics, Emory University, Alanta, GA, United States
1Diagnostic Radiology, Emory University, Lilburn, GA, United States, 2Neurosurgery, Emory University, Atlanta, GA, United States, 3College of Medicine, Emory University, Atlanta, GA, United States, 4Biostatistics and Bioinformatics, Emory University, Alanta, GA, United States
Synopsis
Keywords: Tumors, Surgery
Preoperative diffusion tensor imaging (DTI) data was analyzed using Automated Fiber Quantification (AFQ) along the corticospinal tract (CST) for 58 patients undergoing surgical resection of primary or metastatic brain lesions. For each patient, DTI parameters were analyzed along the ipsilateral CST, the side of the pathological lesion, and the contralateral CST, the side opposite the pathological lesion. Patients were then separated based on the presence or absence of postoperative motor weakness. Patients with post operative motor weakness were found to have significantly different diffusion parameters along their ipsilateral CST compared to the ipsilateral CST of patients without postoperative motor weakness.Introduction
Postoperative motor weakness is a significant clinical endpoint affecting the quality of life of patients undergoing neurosurgery for the resection of brain lesions. Development of prognosticators for postoperative motor weakness using non-invasive preoperative neuroimaging data could significantly affect preoperative planning and clinical decision making.Methods
Preoperative neuroimaging data including diffusion tensor imaging (DTI) and anatomic T1-weighted MRI was retrospectively analyzed for 58 patients from the CNS Tumor Outcome Registry at Emory (CTORE) database, which includes patients with primary (n=46, 79.3%) or metastatic brain lesions (n=12, 20.7%). All patients underwent surgery for resection of their brain lesion and postoperative motor outcomes were assessed clinically based on the absence or presence of postoperative motor weakness, which could range from mild focal weakness to motor paralysis.To analyze the motor pathways, the bilateral corticospinal tract (CST) for each patient was automatically extracted from the DTI data using Automated Fiber Quantification (AFQ)1 from predefined anatomic landmarks. Along-the-tract profiles were generated for each patient for the ipsilateral CST, the side with the primary lesion, and the contralateral CST, the side opposite the primary lesion. Conventional DTI parameters were analyzed including mean diffusivity (MD) and fractional anisotropy (FA). The tract profiles were assessed both qualitatively and quantitatively. Statistical analysis of the ipsilateral CST for patients with and without postoperative motor weakness was performed using hierarchical linear models (HLM). Additionally, the average value of the ipsilateral and contralateral CST for each patient was computed by averaging MD and FA along the entire tract profile. Tract profiles from the contralateral CST of all patients was included for qualitative comparison.
Results
Following surgical resection of their brain lesions, 35 patients had postoperative motor weakness (60%) and 23 patients had no motor weakness (40%). Example neuroimaging data from a patient with a primary glioblastoma and postoperative motor weakness is demonstrated in Figure 1. Tract profiles for the patient in Figure 1 with postoperative motor weakness are demonstrated in Figure 2 for the ipsilateral and contralateral CST. Tract profiles for the ipsilateral and contralateral CST for an example patient without postoperative motor weakness are demonstrated in Figure 3. Average parameter values over the entire CST for patients with and without motor weakness are provided in Figure 4.The average MD for patients with postoperative motor weakness was 0.802 +/- 0.089 in the ipsilateral CST and 0.747 +/- 0.039 in the contralateral CST, and the average MD for patients without postoperative motor weakness was 0.754 +/- 0.065 in the ipsilateral CST and 0.733 +/- 0.044 in the contralateral CST. The average FA for patients with postoperative motor weakness was 0.527 +/- 0.083 in the ipsilateral CST and 0.597 +/- 0.046 in the contralateral CST, and the average FA for patients without postoperative motor weakness was 0.572 +/- 0.061 in the ipsilateral CST and 0.595 +/- 0.044 in the contralateral CST. Using HLM, patients with postoperative motor weakness had significantly increased MD (p = 0.020) and significantly decreased FA (p=0.026) along their ipsilateral CST.
Discussion
AFQ is a fully automated neuroimaging technique which can be used to analyze white matter pathways from conventional clinical neuroimaging data based on predefined anatomical landmarks which helps standardize the tract profiles between patients and facilitates individual and group-wise comparison.Increased MD and decreased FA along white matter pathways in patients with brain lesions could indicate preoperative pathological involvement as MD can be a surrogate marker for edema, FA can be a surrogate marker for tissue microstructure and white matter alignment, and white matter involvement of brain lesions would be hypothesized to increase vasogenic edema (increase MD) and decrease white matter microstructure and the organization of fiber bundles (decrease FA). Although white matter involvement can also be assessed qualitatively from conventional neuroimaging techniques including T2-FLAIR and clinical DTI, AFQ provides fully automated and quantitative technique for along-the-tract analysis of specific white matter pathways, which decreases inter- and intra-observer variability and could provide functionally meaningful, quantitative prognosticators.
Conclusion
Patients who experienced postoperative motor weakness following surgical resection of brain lesions demonstrated increased MD and decreased FA along the ipsilateral CST, which could indicate pathological involvement of the primary motor pathway prior to surgery, placing patients at higher risk of experiencing postoperative motor weakness. Knowing which patients are likely to have postoperative motor weakness in advance could provide valuable information to help surgeons and patients in preoperative planning and clinical decision making. This work demonstrates possible fully automated prognosticators of motor outcomes and corollaries for preoperative planning.Acknowledgements
No acknowledgement found.References
1. Yeatman JD, Dougherty RF, Myall NJ, Wandell BA, Feldman HM. Tract profiles of white matter properties: automating fiber-tract quantification. PloS One, 7: e49790.Figures

Figure 1: Example MRI data for a patient with
right-sided primary glioblastoma who experienced postoperative motor weakness.
(A) T2-FLAIR, (B) T1-weighted MPRAGE, (C) Mean Diffusivity (MD) map from DTI
and (D) Fractional Anisotropy (FA) map from DTI. (E) The bilateral CST for this
patient are extracted using AFQ and tract profiles are computed along the
tracts from caudal to crainal using the MD and FA maps.
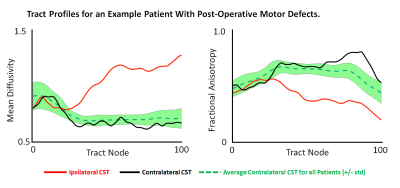
Figure 2: MD and FA tract
profiles for an example patient with postoperative motor weakness (shown in
Figure 1) for the ipsilateral (red) and contralateral (black) CST. The average
tract profile for the contralateral CST for all patients (+/- std) is shown in
green for reference. Tract nodes are evenly spaced nodes, interpolated along
the CST with predefined anatomic landmarks at its caudal (0) and cranial (100)
extent, which are standardized between patients.
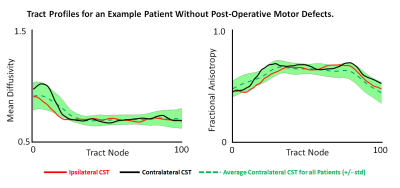
Figure3: MD and FA tract profiles for an example patient who did
not experience postoperative motor weakness for the ipsilateral (red) and
contralateral (black) CST. The average tract profile for the contralateral CST
for all patients (+/- std) is shown in green for comparison. Tract nodes are
evenly spaced nodes, interpolated along the CST with predefined anatomic
landmarks at its caudal (0) and cranial (100) extent, which are standardized
between patients.
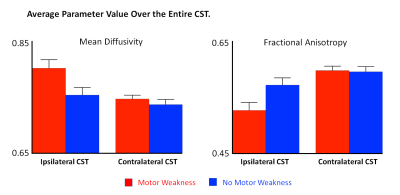
Figure 4: Average
parameter value along the ipsilateral and contralateral CST for patints with
and without postoperative motor weakness (+/- standard error) for mean
diffusivity and fractional anisotropy.
DOI: https://doi.org/10.58530/2023/2127