2104
The Relationship between MR Imaging Characteristics of Bilateral Carotid High-risk Plaques and Recurrence of Stroke
Ruijing Xin1, Maoxue Wang1, and Bing Zhang1
1Department of Radiology, The Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China
1Department of Radiology, The Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China
Synopsis
Keywords: Stroke, Atherosclerosis, High-risk plaque
Carotid HRP is one of the major sources of ischemic stroke. Recent studies have focused on identifying characteristics of HRP which is defined as lesion with IPH, FCR, or LRNC. We compared the plaque characteristics of patients with bilateral carotid HRPs between patients with recurrent stroke and those without recurrent stroke using MR vessel wall imaging. We determined the association between HRP plaque features and recurrent stroke in patients with bilateral carotid HRPs. We found that those with larger plaque burden, more juxta luminal IPH and/or thrombus, and juxta luminal calcification in HRPs were more likely to have recurrent stroke.Introduction
Carotid high-risk atherosclerotic plaque (HRP) is one of the major sources of ischemic stroke 1. Recent studies have focused on identifying characteristics of HRP which is defined as lesion with intraplaque hemorrhage (IPH), fibrous cap rupture (FCR), or large lipid rich necrotic core (>40%) (LRNC) 2. To compare the plaque characteristics between patients with and without recurrent stroke in patients with bilateral carotid HRPs using MR vessel wall imaging. The relationship between HRPs characteristics and recurrent stroke was also determined.Method
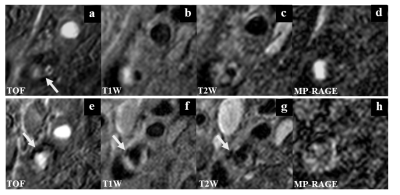
Study sample: Patients with recent symptomatic carotid plaques determined by ultrasound were included. The exclusion criteria included: 1) cardioembolic stroke; 2) hemorrhagic stroke; 4) history of radiation therapy in the neck; 5) claustrophobia; or 6) contraindication to MR examination. Clinical information collection: Clinical characteristics including age, gender, body mass index (BMI), smoking, blood pressure, hypertension, hyperlipidemia, levels of TC, HDL, LDL, and TG, diabetes, family history of cardiovascular disease, history of coronary heart disease, antihypertensive or statin therapy were collected. MR imaging: The carotid artery vessel wall was imaged by multicontrast imaging protocol including 3D TOF, 2D T1W and T2W, and 3D MP-RAGE sequences with the following parameters: TOF: FFE, TR/TE 20/4.9 ms, slice thickness 1 mm; T1W: TSE, TR/TE 800/10 ms, slice thickness 2 mm; T2W: TSE, TR/TE 4800/50 ms, slice thickness 2 mm; and MP-RAGE: FFE, TR/TE 8.8/5.3 ms, slice thickness 1 mm. All sequences were acquired with the same FOV of 14×14 cm2 and matrix size of 256×256. Image analysis: Two experienced radiologists independently analyzed the MR images blinded to clinical information with consensus. Carotid plaque was characterized by eccentric wall thickening on MR vessel wall images. The presence / absence LRNC, IPH, and FCR was assessed using published criteria 3. Statistical analysis: Independent sample t test, Mann-Whitney U test or Chi-square test were used to compare the differences of MR image characteristics of HRPs between recurrent group and non-recurrent group. Multivariate Logistic regression was used to analyze the relationship between MR imaging characteristics of HRP and recurrent stroke after adjusting confounding factors.Results
A total of 71 subjects (mean age: 66.4±7.3 years, 66 males) with recent stroke or TIA (within 2 weeks after onsets of symptoms) and bilateral carotid HRPs were included and underwent carotid MR vessel wall imaging. Compared the HRPs in non-recurrent stroke group, HRPs in recurrent stroke group showed greater WT (P = 0.010), NWI (P = 0.003) and stenosis (P = 0.001). HRPs in recurrent stroke group had significantly higher prevalence of juxta luminal IPH and/or thrombus (52.6% vs. 19.2%; P = 0.006) and juxta luminal calcification (42.1% vs. 9.6%; P = 0.004). After adjusted for age, gender and BMI. mean NWI (OR: 1.12, 95% CI: 1.03-1.21, P = 0.008), luminal stenosis (OR: 1.04, 95% CI: 1.02-1.07, P = 0.001), juxta luminal IPH and/or thrombus (OR: 5.15, 95% CI: 1.59-16.63, P = 0.006), and juxta luminal calcification (OR: 9.35, 95% CI: 2.24-38.94, P = 0.002) were found to be associated with recurrent stroke. After further adjusted for NWI and luminal stenosis, juxta luminal IPH and/or thrombus (OR: 5.33, 95%CI: 1.30-21.83, P = 0.020) and juxta luminal calcification (OR: 7.70, 95%CI: 1.37-43.22, P = 0.020) showed significant association with recurrent stroke (Fig. 1).Discussion and conclusion
For patients with bilateral carotid HRPs, those with larger plaque burden, more juxta luminal IPH and/or thrombus, and juxta luminal calcification in HRPs were more likely to have recurrent stroke.Acknowledgements
None.References
1. Seeger JM, Barratt E, Lawson GA, et al. The relationship between carotid plaque composition, plaque morphology, and neurologic symptoms. J Surg Res. 1995 Mar;58(3):330-336.2. Underhill HR, Hatsukami TS, Cai J, et al. A noninvasive imaging approach to assess plaque severity: the carotid atherosclerosis score. AJNR Am J Neuroradiol. 2010 Jun;31(6):1068-1075.
3. Cai JM, Hatsukami TS, Ferguson MS, et al. Classification of human carotid atherosclerotic lesions with in vivo multicontrast magnetic resonance imaging. Circulation. 2002 Sep 10;106(11):1368-1373.
DOI: https://doi.org/10.58530/2023/2104