2093
Association of longitudinal changes in cerebral microstructure with cognitive function in breast cancer survivors after adjuvant chemotherapy1Department of Medical Imaging and Radiological Sciences, and Department of Artificial Intelligence, Chang Gung University, Taoyuan, Taiwan, 2School of Medicine, Chang Gung University, Taoyuan, Taiwan, 3Department of Psychiatry, Chang Gung Memorial Hospital, Chiayi, Taiwan, 4Department of Diagnostic Radiology, Chang Gung Memorial Hospital, Chiayi, Taiwan, 5Medical Imaging Research Center, Institute for Radiological Research, Chang Gung University and Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan
Synopsis
Keywords: Neuroinflammation, Cancer
Adjuvant chemotherapy for breast cancer might impact cognitive function and brain structure. In this study, we investigated the cerebral microstructural changes in breast cancer survivors after adjuvant chemotherapy and the correlation with cognitive function with longitudinal study designs. The results showed brain volume reduction in thefrontal and temporal regions were also observed in patients from baseline to postchemotherapy. An association between brain volume and cognitive performance was also found in the limbic system. According to our findings, the study was useful in developing a prediction model as well as a guide for cancer treatment.Introduction
The most common cancer diagnosis among women and the most common cause of death from cancer among women globally is breast cancer. Chemotherapy is the most commonly used treatment method for cancer. Moreover, a significant proportion of cancer patients with chemotherapy experience cognitive dysfunction, which is also known as chemotherapy-induced cognitive impairment (CICI), which results in poor quality of life for these patients [1-3]. In this study, we used a longitudinal study design to investigate brain structural changes in breast cancer survivors. The aim of this study was to explore (1) whether any changes in brain volume and shape were observed between baseline and time point 2 in breast cancer patients; and (2) whether neuropsychological performance was associated with brain volume changes in patients with breast cancer.Methods
All participants underwent structural MRI. We first recruited 67 prechemotherapy patients (BB), and 77 healthy controls (BH) from the Chiayi Chang Gung Memorial Hospital. For the follow-up study, 28 participants in the BH and 28 in the BB groups returned for imaging and assessment (BHF, BBF). Each participant completed the Patient Health Questionnaire-9 (PHQ-9) to evaluate depression and the Hospital Anxiety and Depression Scale-Anxiety (HADS-A) to evaluate anxiety. For the longitudinal analysis, measures used in the study included MRI scans of the brain and cognitive assessments. These were completed after the patients were recruited (t1) and after they completed chemotherapy (t2). An average time interval of 6-7 months followed the completion of chemotherapy. The healthy controls were also evaluated at the matched time interval. BB and BBF groups also conducted the following cognitive assessments: the Color Trails test (CCT), digit symbol substitution subtest (DSS) of the Wechsler Adult Intelligence Scale, and FACT-Cog.In all participants, the T1-weighted images were acquired on a 3 T MRI scanner (Verio, Siemens, Germany). Brain MRI was performed in the magnetization prepared rapid gradient echo (MPRAGE) sequence. Voxel-based morphometry analysis was performed to evaluate differences in brain volume [4]; vertex-based shape analysis was used to assess the shape alterations of subcortical regions [5]. Moreover, multiple regression was applied to assess the association between the changes in neuropsychological assessment and brain volume.
Results
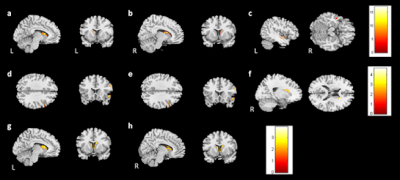
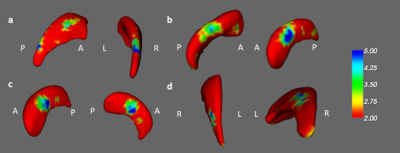
In the voxel-based morphometry (group-by-time interaction), the bilateral caudate and left middle temporal gyrus showed differing brain volumes between healthy control and prechemotherapy patients from t1 to t2 (Fig. 1a-c). Furthermore, the right inferior frontal gyrus and right superior temporal gyrus volumes were reduced in the BBF group compared with the BB group (Figure 1d, 1e). However, the BBF group had a greater volume increase in the right caudate (Figure 1f). Additionally, we found that the bilateral caudate volume was reduced in the BHF group compared to the BH group (Figure 1g, 1h).In the vertex-based shape analysis, a comparison of the healthy controls and prechemotherapy patients revealed differences in caudate and hippocampal shapes on the left side (Figure 2a, 2b). Additionally, paired t tests revealed a difference in the shape of the left hippocampus between the BB and BBF groups (Figure 2c). A difference in the shape of the right caudate was found between the BH and BHF groups (Figure 2d).
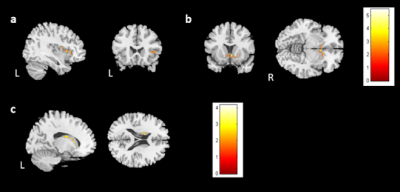
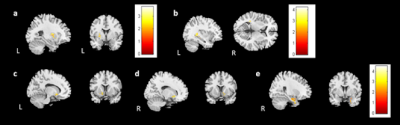
We also analyzed the association between brain volume change and cognitive performance or mood symptoms for 28 participants from the BB group. The outliers were ruled out in the analysis. In the analysis, the HADS-A was negatively associated with gray matter volume changes in the right insula and bilateral caudate (Figure 3a, 3b). The analysis did not find a significant association between brain volume change and PHQ-9. For the evaluations of cognitive performance, a decrease in DSS scores was associated with reduced white matter volume in the left caudate (Figure 3c). CTT1 and CTT2 did not show any significant association with brain volume changes. In subjective cognitive assessments, there was an association between decreased FACT-Cog and reduced white matter volume in the left putamen (Figure 4a). Furthermore, the analysis identified a positive association between perceived cognitive impairment and volume changes in the left temporal gyrus (Figure 4b). Perceived cognitive abilities were also positively associated with volume changes in thebilateral putamen and left parahippocampus (Figure 4c-e).
Discussion
In this study, brain volume and shape differences were investigated longitudinally in patients with breast cancer, as well as the interaction of brain volume changes with cognitive performance. In the longitudinal studies, we observed changes in the caudate, frontal, and temporal areas. In addition, association analysis revealed a significant correlation between certain brain volumes and neuropsychological assessments.Conclusion
Our longitudinal results suggest that chemotherapy may result in a volume reduction in breast cancer survivors. Moreover, we found that the brain volume of certain regions was associated with cognitive performance. These results suggest that structural neuroanatomical correlates may exist and affect cognitive impairment before and after chemotherapy. Based on our findings, we could offer a better understanding of the cerebral structural changes in breast cancer survivors, establish a subsequent prediction model, and serve as a reference for subsequent treatment.Acknowledgements
This study was supported by research grants MOST107-2221-E-182-054-MY3 and NSTC111-2221-E-182-021 from the National Science and Technology Council, Taipei, Taiwan, respectively. This study was also supported by grantsNMRPD1H0101~3 from Chang Gung University, Taoyuan, Taiwan and CORPG6G0101~3 and CORPG6G0121~3 from Chang Gung Memorial Hospital, Chiayi, Taiwan.References
1. Janelsins M.C., et al., Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int Rev Psychiatry 2014, 26(1):102-113.
2. Ahles T.A., et al., Longitudinal assessment of cognitive changes associated with adjuvant treatment for breast cancer: impact of age and cognitive reserve. J Clin Oncol 2010, 28(29): 4434-4440.
3. Wefel J.S., et al., Acute and late onset cognitive dysfunction associated with chemotherapy in women with breast cancer. Cancer 2010, 116(14): 3348-3356.
4. Kurth F., et al., Voxel-Based Morphometry. In: Brain Mapping. edn. Edited by Toga AW. Waltham: Academic Press; 2015: 345-349.
5. Patenaude B., et al., A Bayesian model of shape and appearance for subcortical brain segmentation. Neuroimage 2011, 56(3): 907-922.
Figures