2092
The diagnostic value of TSE-DWI in patient with Benign paroxysmal positional vertigo (BPPV): a feasibility study1The First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, China, 2Philips Healthcare, Xi'an, China
Synopsis
Keywords: Head & Neck/ENT, Diffusion/other diffusion imaging techniques, Benign paroxysmal positional vertigo, turbo spin-echo diffusion weighted imaging
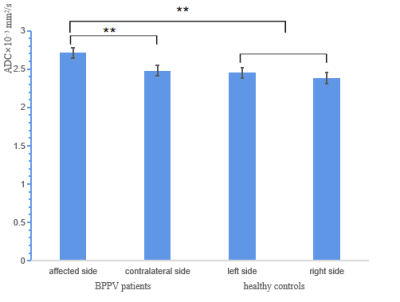
This study explored the feasibility of TSE-DWI in inner ear and determined the diagnostic accuracy and interobserver performance of TSE-DWI in BPPV. The method is to evaluate the difference of ADC values between benign paroxysmal positional vertigo (BPPV) patients and healthy controls. Our research shows that The ADC values of semicircular canal in the BPPV patients (affected side) were higher than that of the contralateral ear. Moderate diagnostic accuracy of DWI was seen in the diagnosis of BPPV. Therefore, we consider that the TSE-DWI derived ADC value may represent promising novel imaging markers of inner ear disease.Introduction
Benign paroxysmal positional vertigo (BPPV) is the most common cause of vertigo worldwide1. The cause of BPPV remains unclear. Recent high-resolution magnetic resonance imaging (HR-MRI) studies have reported morphological abnormalities in the inner ear of patients with intractable BPPV2,3. Diffusion weighted imaging (DWI), which can noninvasively detect the diffusion of water molecules in tissues, provides specific image contrast about tissue microstructure. Now DWI is commonly a routine MRI sequences in daily clinical diagnosis, and the DWI derived apparent diffusion coefficient (ADC) map has been a quantitative measurement for various applications outside the central nervous system4. However, due to the small size and the complicated tissue boundaries of the inner ear, the results of the conventional echo planar imaging DWI (EPI-DWI) become terrible. Compared with EPI-DWI, Single shot turbo spin-echo DWI (TSE-DWI) has fewer susceptibility artifacts and higher signal-to-noise ratio. And it is suitable for inner ear diffusion imaging. Therefore, the aim of this study is to explore the feasibility of TSE-DWI in inner ear and determine the diagnostic accuracy and interobserver performance of TSE-DWI in BPPV.Methods
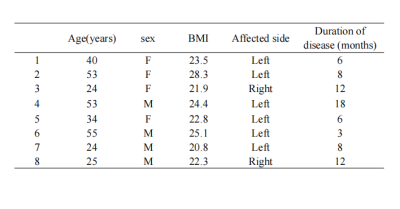
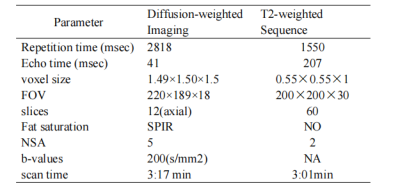
In this study,bilateral inner ear of 8 healthy controls (4 men, 4 women; mean age 34.2 years, range 23–46 years) and bilateral inner ear of 8 BPPV patients (8 affected ears, 8 healthy ears; 4 men and 4 women; mean age 38.5 years, range 24–53 years) were collected (Table 1). All participants underwent MR examinations on a 3.0T MR scanner (Ingenia CX, Philips, the Netherlands) by using 32-channel phase array head coil. TSE-DWI and T2W with a scan range from the superior border of the petrous bone to the inferior border of the mastoid process were performed. Further sequence details are summarized in Table 2. All the obtained images were transferred to Philips IntelliSpace Portal workstation for post-processing. Apparent diffusion coefficient (ADC) values of semicircular canal (SC) were then measured. The user defined three region-of-interests (ROIs) were manually drawn on DWI images independently by two experienced radiologists with 5 and 6 years of experience in clinical MR interpretation, respectively. The average of results was used for further analysis. Inter-reader agreement of the ADC values was assessed by using intraclass correlation coefficient (ICC). Levene’s test was performed to evaluate the equality of variances. The difference of ADC values of the two groups were evaluated by two sample t-test. SPSS (version 25) was used for statistical analysis. P<0.05 was set to indicate statistically significant difference. Receiver operating characteristic (ROC) analysis was performed for ADC values.Results
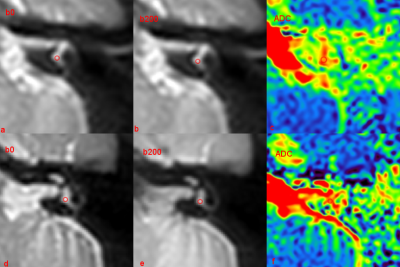
Figure 1 showed the typical examples of inner ear DWI images and corresponding ROI placement. ICCs for intra-reader agreement of ADC measurements were 0.95. No differences in the ADC values of SC were detected between the left ear and the right ear of healthy volunteers (left side: 2.38±0.10 ×10−3 mm2/s, right side: 2.45±0.17 ×10−3 mm2/s, P>0.05). The ADC values of SC in the affected ear were higher than that of the contralateral ear (affected ear: 2.71±0.18 ×10−3 mm2/s, contralateral ear: 2.48±0.16 ×10−3 mm2/s, p < 0.05) (Figure2). Moderate diagnostic accuracy of DWI was seen in the diagnosis of BPPV (AUC=0.841).Discussion
In this study, we found that the TSE-DWI is advisable for intractable BPPV. Though EPI is the well-established DWI technique, it is susceptible to artefacts easily produced by the non-uniform magnetic field of the temporal bone region. We therefore choose TSE-DWI to reduce geometric distortions and signal loss. Our study used the modulus averaging method, short RFpulses, and SENSE, which resulted in a shorter TE, higher SNR, and reduced image blurring. Previous study applied the sequence in the evaluation of tumors of the head and neck, and their results shows TSE-DWI produced better quality images than EPI-DWI5. The ADC value reflects the true quantification of molecules diffusion coefficient, which is an index that indirectly evaluates the size of diffusion barrier such as cell membrane or myelin sheath. Our study demonstrates the BPPV patients showed a significant increase in ADC values which may be caused by changes in perilymph and endolymph of the inner ear. House and Honrubia proposed in the established BPPV model: otoconia need to reach a significant level (if the individual particles have dimensions of approximately 10 microns, the volume of particles predicted in the cupulolithiasis model corresponds to a number of particles in the order of 490, and for the canalithiasis model, approximately 62 otoconiathe number of earstones), it will affect the flow of the endolymph, and the symptoms of BPPV will occur6. We found the diffusion alterations in the SC of BPPV patients, which may be related to the abnormality of endolymph components.Conclusion
In DWI, an ideal standard TSE-DWI protocol in inner ear is suggested instead of EPI-DWI. The ADC value of SC in the BPPV group were significantly higher than the control group. The TSE-DWI derived ADC value may represent promising novel imaging markers of inner ear disease.Acknowledgements
No acknowledgement found.References
1. Kim HJ, Park J, Kim JS. Update on benign paroxysmal positional vertigo. J Neurol. 2021 May;268(5):1995-2000. doi: 10.1007/s00415-020-10314-7.
2. Dallan I, Bruschini L, Neri E, et al. The role of high-resolution magnetic resonance in atypical and intractable benign paroxysmal positional vertigo: our preliminary experience. ORL J Otorhinolaryngol Relat Spec 2007;69:212Y7.3.
3. Horii A, Kitahara T, Osaki Y, Imai T, Fukuda K, Sakagami M, Inohara H. Intractable benign paroxysmal positioning vertigo: long-term follow-up and inner ear abnormality detected by three-dimensional magnetic resonance imaging. Otol Neurotol. 2010 Feb;31(2):250-5. doi: 10.1097/MAO.0b013e3181cabd77.
4. Thoeny HC, De Keyzer F. Extracranial applications of diffusion-weighted magnetic resonance imaging. Eur Radiol 2007; 17:1385–1393.
5. Panyarak W, Chikui T, Yamashita Y, Kamitani T, Yoshiura K. Image Quality and ADC Assessment in Turbo Spin-Echo and Echo-Planar Diffusion-Weighted MR Imaging of Tumors of the Head and Neck. Acad Radiol. 2019 Oct;26(10):e305-e316. doi: 10.1016/j.acra.2018.11.016.
6. Sugita-Kitajima A, Azuma M, Hottori K, et al. Evaluation of the otolith function using sinusoidal off-vertical axis ratation in patients with benign paroxysmal positional vertigo[J]. Neurosci Lett, 2007, 422(1): 81-86.
Figures