2088
DWI Imaging for the Discrimination of Cytotoxic Lesions and Acute Ischemic Infarction of the Corpus Callosum: Utility of Relative ADC.1Department of Radiology, Xijing Hospital, Fourth Military Medical University, Xi'an, China
Synopsis
Keywords: Head & Neck/ENT, Diffusion Tensor Imaging
Cytotoxic lesions of the corpus callosum (CLOCCs) is a rare clinical-imaging syndrome, which is difficult to differentiate from acute ischemic infarction of the splenium of the corpus callosum (AII-SCC) by conventional MRI, DWI and ADC value. In this study, a novel relative ADC (rADC) value was proposed. Results showed that the rADC value of CLOCCs is significantly lower than that of AII-SCC, which Indicated that rADC value may have the potential to distinguish these two diseases.ABSTRACT
IntroductionCytotoxic lesions of the corpus callosum (CLOCCs) is a rare clinical-imaging syndrome characterized by secondary diffusion-restricted lesions of the splenium of the corpus callosum (SCC) and lack of clinical specificity [1]. The main cause of acute ischemic infarction of SCC (AII-SCC) is acute cerebrovascular accident on the basis of atherosclerosis [2]. Since the corresponding clinical symptoms of nerve injury in the infarct site often occur in SCC and brain simultaneously [3-4], it is difficult to distinguish the CLOCCs and AII-SCC according to the clinical features. CLOCCs had characteristic MRI imaging findings, including round/quasi round/boomerang lesions with uniform signal and single splenium of the corpus callosum, symmetrical distribution in the midline of the central region, clear boundary, no edema occupying, no enhancement. However, at the initial diagnosis, the MRI signals were similar to those of All-SCC [5]. Relative ADC (rADC) value is defined to optimize ADC value and has been reported to be abnormal in many diseases, such as Glioblastoma, pancreatic cancer and breast masses [6-8]. Thus, in this study, we would evaluate whether the rADC can identify between CLOCCs and AII-SCC in adults.
Methods
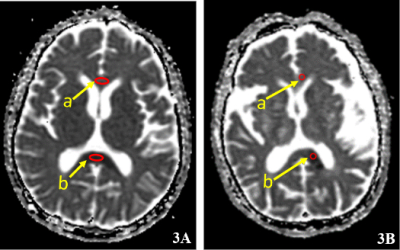
A total of 71 patients with CLOCCs, aged 15-69 years (mean, 35.8±14.4 years), and 88 patients with AII-SCC, aged 18-88 years (mean, 55.5±14.2 years), were retrospectively collected. A GE Discovery MR750 3.0T scanner and a 16-channel head phased-array coil were used. The cranial MRI sequences and scan parameters were as follows: T1WI (TR = 1800 ms, TE = 20 ms); T2WI (TR = 4700 ms, TE = 110 ms); T2-FLAIR (TR = 8500 ms, TE = 150 ms) and DWI (TR = 4500 ms, TE = 82 ms, b values of 0 and 1000 s/ mm2). All patients' images were transferred to the post-processing workstation, and the main observations were lesion location, number, morphology, and signal characteristics. The ADC values of SCC lesions were measured by hand-drawing and the region of interest (ROI) was selected as the largest level of the lesion for each patient. The ROI was placed in the center of the selected lesion with the area of each greater than 15 mm2 and edge greater than 3 mm from the edge of the lesion. The ADC values of all lesions were measured three times and averaged as the final results. The ADC values at the center of the largest level of the genu of the corpus callosum (GCC) were measured simultaneously for all patients using the same method, and the rADC values were calculated as (ADCGCC - ADCSCC) /ADCGCC. Two samples t-test or non-parametric test were used to compare the ADCGCC, ADCSCC and rADC value between CLOCCs and SCC groups when these three values satisfy the normal distribution or not, respectively.
Results
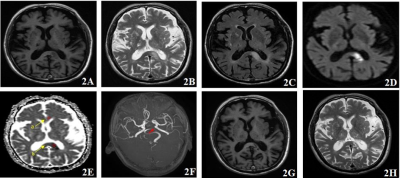
71 patients with CLOCCs showed equal/low signal intensity on T1WI, high signal intensity on T2WI, FLAIR and DWI and low signal intensity on ADC during MRI plain scan (FIG. 1), and 88 patients with AII-SCC showed similar results with CLOSSs (FIG. 2). No significant differences were found in ADCSCC and ADCGCC value between CLOCCs and AII-SCC groups (0.8651±0.6460 vs 0.8179±0.5937 x10-3mm2/s, p=0.635 and 1.2088±0.6317 vs 1.2874±0.6473 x10-3mm2/s, p=441 for ADCSCC and ADCGCC, respectively). The rADC value in CLOCCs group was significantly lower than the one of AII-SSC group (0.3511±0.1931 vs 0.4212±0.1737 x10-3mm2/s, p=0.019, FIG3).
Discussion
It is generally believed that the lesion is irreversible when the DWI sequence presents the diffusion limited signal caused by cytotoxic edema [9]. Although MRI signal of CLOCCs group showed similar with the one of AII-SCC group (no significant differences of ADCSCC and ADCGCC values between the two groups), the lesion is reversible in CLOSSs group, indicating that the pathogenic mechanism of the two diseases is not completely consistent. In this study, the rADC value of the two groups were calculated in an innovative way, and we found that the rADC value of CLOCCs lesions were lower than those of AII-SCC. We speculated that it may be related to its etiology and pathogenesis: most CLOCCs develop suddenly without other chronic underlying diseases, while AII-SCC in such patients has higher sensitivity to pathogenic factors, more obvious injury response, and lower ADC value.
Conclusion
The proposed new relative ADC value strategy that derived from DWI could greatly improve the diagnostic performance for the cytotoxic lesions of the corpus callosum and acute ischemic infarction of the splenium of the corpus callosum in adults.
Acknowledgements
No acknowledgement found.References
[1] Starkey J, Kobayashi N, Numaguchi Y, et al. Cytotoxic Lesions of the Corpus Callosum That Show Restricted Diffusion: Mechanisms, Causes, and Manifestations. Radiographics 2017;37: 562-576.
[2] Takahashi Y, Hayakawa I, Abe Y. Diagnostic odyssey of acute disseminated encephalomyelitis in children. Sci Rep 2021;11: 21954.
[3] Lischke A, Domin M, Freyberger HJ, et al. Structural Alterations in the Corpus Callosum Are Associated with Suicidal Behavior in Women with Borderline Personality Disorder. Front Hum Neurosci 2017;11: 196.
[4] Li S, Sun X, Bai YM, et al. Infarction of the corpus callosum: a retrospective clinical investigation. PLoS One 2015;10: e0120409.
[5] Bagatti D, Messina G. Cytotoxic Lesion in the Splenium of Corpus Callosum Associated with Intracranial Infection After Deep Brain Stimulation. World Neurosurg 2020;135: 306-307.
[6] Feng A, Yuan P, Huang T, et al. Distinguishing Tumor Recurrence From Radiation Necrosis in Treated Glioblastoma Using Multiparametric MRI. Acad Radiol 2022;29: 1320-1331.
[7] Yilmaz E, Sari O, Yilmaz A, et al. Diffusion-Weighted Imaging for the Discrimination of Benign and Malignant Breast Masses; Utility of ADC and Relative ADC. J Belg Soc Radiol 2018;102: 24.
[8] Nishiofuku H, Tanaka T, Marugami N, et al. Increased tumour ADC value during chemotherapy predicts improved survival in unresectable pancreatic cancer. Eur Radiol 2016;26: 1835-42.
[9] Osa GA, Brambati SM, Desautels A, et al. Timing stroke: A review on stroke pathophysiology and its influence over time on diffusion measures. J Neurol Sci 2022;441: 120377.
Figures