2082
Association of Plaque Characteristics, Pial Collaterals and Perfusion with Recurrent Ischemic Stroke in Middle Cerebral Artery Stenosis1Department of Radiology, Zhongda Hospital, Medical School, Southeast University, Nanjing, China, 2Philips Healthcare, Shanghai, China
Synopsis
Keywords: Stroke, Atherosclerosis
Association between plaque characteristics, perfusion, pial collaterals (PCs) and recurrent ischemic stroke is unclear. Few analyses focus on combination of blood vessels, perfusion and PCs. In this study, 62 patients presenting with a transient ischemic attack or acute ischemic stroke caused by middle cerebral artery atherosclerosis were involved. All patients underwent the routine head MRI/MRA scan and high-resolution vessel wall imaging examinations. We performed a comprehensive assessment of plaque characteristics, perfusion and PCs. We concluded that brain perfusion and PCs are correlated with recurrence of ischemic stroke and their combination provided incremental value in identifying the recurrence of ischemic stroke.
INTRODUCTION
Intracranial atherosclerotic disease (ICAD) represents the most common cause of ischemic stroke across the world1. ICAD has a higher tendency to occur in the middle cerebral artery especially in Asians2. Patients with ICAD have increased risk of recurrent stroke3.With the development of high-resolution vessel wall imaging (HR-VWI), more and more attention has been paid to not only the degree of vessel stenosis but also plaque characteristics of ICAD. However, previous studies mostly focused on the plaque features in ischemic stroke. There were few studies in which the analysis of plaque feature, perfusion and pial collaterals (PCs) were all presented4. In this study, we aim to investigate plaque characteristics, perfusion and PCs in recurrent ischemic stroke and demonstrate the value of these factors in the identification of the recurrence of ischemic stroke.METHODS
From February 2018 to July 2021, patients presenting with a transient ischemic attack (TIA) or acute ischemic stroke(AIS) caused by unilateral atherosclerotic middle cerebral artery (MCA) stenosis(>50%) who underwent the routine head MRI/MRA scan,HR-VWI and dynamic susceptibility contrast-enhanced perfusion weighted imaging on an 3.0T MRI scanner(Ingenia 3.0T, Philips Healthcare, Best, the Netherlands) at Zhongda Hospital affiliated Southeast University were recruited. Based on the results of a twelve-month telephone follow-up, 62 patients were divided into group with recurrence (n=12) and group without recurrence (n=50). For all patients, the evaluation of characteristics of culprit plaques (defined as the only lesion or the most stenotic lesion when multiple plaques were present within the same vascular territory of the stroke), PCs and brain perfusion were performed. Plaque characteristics include stenosis grade, lumen area of stenotic lesion (LAlesion), plaque area, plaque length, standardized wall index (NWI), eccentricity index, remodeling index, and plaque enhancement grade. PCs within the territory of stenotic MCA was evaluated on axial time-of-flight magnetic resonance angiography (TOF-MRA) source images on the level of lateral ventricle body according to a grading system: grade 0, absent vascular signal; grade 1,collaterals<50% compared to the reference side; grade 2,collaterals ≥50% compared to the reference side; grade 3, collaterals equal to or more than the reference side. Brain perfusion within the territory of MCA was visually assessed on a 10-point cerebral blood flow map based on the Alberta Stroke Program Early CT score (CBF-ASPECTS). Each ASPECTS region was scored 0 if abnormal and 1 if normal. Final CBF-ASPECTS for each patient were summed in ten subscores. Plaque features, demographic and clinical characteristics were compared between two groups. Multivariate logistic regression and receiver operating characteristic (ROC) curves were constructed to assess the effect of significant variables alone and their combination on identifying recurrence of ischemic stroke.RESULTS
Table 1 summarized the demographics and plaque characteristics of group with and without recurrence. The CBF-ASPECTS in group with recurrence was 3.33±2.50, which was significantly lower than that in group without recurrence (7.96±1.31, P<0.01). In addition, PCs was significantly different between the two groups (P<0.01). Longer plaque length was seen in the group with recurrence (P<0.01, Table 1, Figure 1-2). The three variables were input for the univariate logistic analysis. Multivariate regression was conducted for the variables with p < 0.05 in the univariate logistic analysis. In addition to plaque length (P=0.06), PCs (P<0.01) and CFB-ASPECTS (P<0.01) were associated with recurrence of ischemic stroke in the univariate logistic analysis. After the adjustment of clinical demographic factors, PCs(P=0.04,OR 0.17,95% 0.03-0.95)and CBF-ASPECTS(P<0.01,OR 0.31,95% 0.14-0.71) remained as significant factors in the multivariate logistic analysis (Table 2). Multivariate logistic analysis revealed that high CBF-ASPECTS and PCs were protective factors for recurrence of ischemic stroke. For the differentiation between group with and without recurrence, the diagnostic accuracy of the combination of CBF-ASPECTS and PCs (95%CI 0.93-1.00, AUC =0.97) was higher than that of CBF-ASPECTS (95%CI 0.82-1.00, AUC =0.92) or PCs (95%CI 0.72-0.94, AUC = 0.83) individually (Figure 3).DISCUSSION
The relationship between plaque length, CBF-ASPECTS, PCs and recurrence of ischemic stroke was observed in our study. A recent study demonstrated that downstream perfusion was valuable in predicting clinical outcomes in ischemic stroke. The mechanism is possibly that hypoperfusion restrict the blood flow's ability to clean emboli and microemboli in distal arteries5. PCs provides alternative blood flow to protect cerebral tissue that is in a hypoperfused state. PCs is relevant to the outcome in acute ischemic stroke patients6. Our finding was similar to the observation from previous studies. Plaque length was significantly different between two groups but failed to remain significant in the multivariate logistic analysis. We speculate that plaque length may play a weaker role than the other factors in identifying recurrent ischemic stroke. Our findings support that a combined assessment of perfusion and collateral circulation may be useful in identifying the recurrence of patients with ischemic stroke.CONCLUSION
Hypoperfusion and poor collateral state independently associated with recurrence of ischemic stroke in patients with atherosclerotic MCA stenosis. The combination of brain perfusion and collateral circulation may play a pivotal role in the identification of recurrent ischemic stroke caused by unilateral atherosclerotic MCA stenosis (>50%).Acknowledgements
No acknowledgement found.References
1. Arenillas JF. Intracranial atherosclerosis: current concepts. Stroke. 2011;42(1 Suppl):S20-S23.
2. Bos D, van der Rijk MJ, Geeraedts TE, et al. Intracranial carotid artery atherosclerosis: prevalence and risk factors in the general population. Stroke. 2012;43(7):1878-1884.
3. Yoon W, Kim SK, Park MS, et al. Endovascular treatment and the outcomes of atherosclerotic intracranial stenosis in patients with hyperacute stroke. Neurosurgery. 2015;76(6):680-686.
4. Liu S, Luo Y, Wang C, et al. Combination of plaque characteristics, pial collaterals, and hypertension contributes to misery perfusion in patients with symptomatic middle cerebral artery stenosis. J Magn Reson Imaging. 2020;51(1):195-204.
5. Lu SS, Ge S, Su CQ, et al. MRI of plaque characteristics and relationship with downstream perfusion and cerebral infarction in patients with symptomatic middle cerebral artery stenosis. J Magn Reson Imaging. 2018;48(1):66-73.
6. Stacey A, Toolis C, Ganesan V. Rates and risk factors for arterial ischemic stroke recurrence in children. Stroke. 2018;49(4):842-847.
Figures
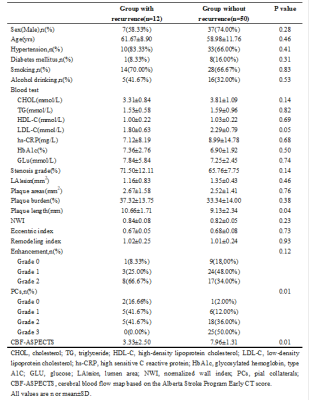
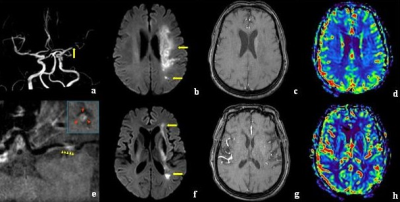
Figure 1. Representative patient with recurrent stroke. A female patient aged 67 with symptoms of right limb weakness for 10 days. (a)On the 3D-TOF MRA, significant stenosis was exhibited in the left M1 segment of MCA(yellow arrow). (b,f)DWI showed hyperintense lesions in left corona radiate and basal ganglia area(yellow arrow). (e)Culprit plaque length(8.43 mm) was measured on postcontrast image of curved reconstruction(yellow arrowheads). (c,g)PCs was grade 1. (d,h)CBF maps showed hypoperfusion areas, involving M1-M6 and internal capsule according to the ASPECTS (socre=3).
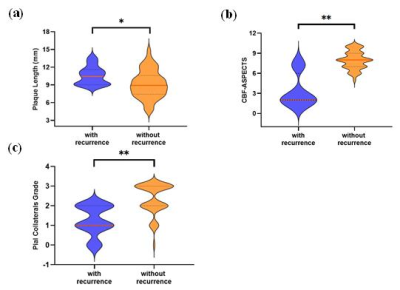
Figure 2. Comparison between groups with and without recurrence in plaque length, CBF-ASPECTS, and PCs between two groups (*P < 0.05, **P < 0.01)
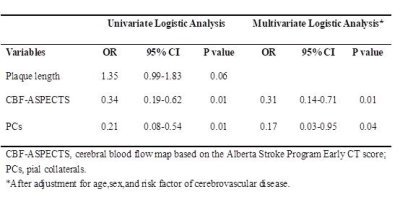
Table 2. Univariate and multivariate logistic analysis for determining the recurrence of ischemic stroke
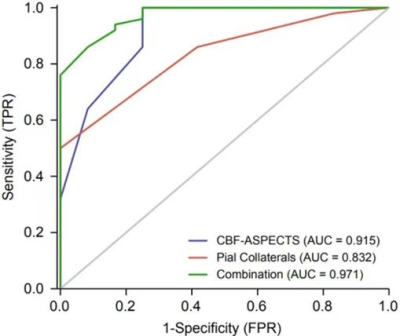
Figure 3. ROC curves for determining the recurrence of ischemic stroke in patient presenting with a transient ischemic attack (TIA) or acute ischemic stroke(AIS) caused by unilateral atherosclerotic middle cerebral artery (MCA) stenosis(>50%). The AUC was 0.915 and 0.832 for CBF-ASPECTS and PCs, respectively.The combination improves the AUC to 0.971, which is higher than any variable alone.