2037
Noninvasive direct assessment of the left gastric vein using 4D flow MRI for risk stratification of esophageal variceal bleeding
Atsushi Higaki1, Yoshihiko Fukukura1, Akihiko Kanki1, Akira Yamamoto1, kazunori Moriya1, and Tsutomu Tamada1
1Radiology, Kawasaki Medical School, Okayama, Japan
1Radiology, Kawasaki Medical School, Okayama, Japan
Synopsis
Keywords: Liver, Liver
This study focused on the feasibility of 4D flow MRI with low-velocity encoding sensitivity as a non-invasive tool for direct estimation of the left gastric vein and stratification of bleeding risk of esophageal varices. Our study showed that the development of esophageal varices was associated with decreased and increased net flow volumes in the left gastric and azygos veins, respectively. These results suggest the promise of 4D flow MRI with low-velocity encoding sensitivity as a non-invasive and accurate method for stratifying the bleeding risk of esophageal varices.INTRODUCTION
Esophageal variceal bleeding is a frequent and life-threatening complication of liver cirrhosis. Endoscopy is considered essential for assessing the severity of esophageal varices; however, most patients have mild esophageal varices without high-risk characteristics. Therefore, non-invasive and reliable methods that allow for risk stratification of esophageal varices would be highly beneficial for patient management. 4D flow MRI, which can provide a detailed assessment of portal vein (PV) system hemodynamics, has the potential to address the major unmet need for non-invasive detection of gastroesophageal varices at high risk for bleeding1. It can replace repeated endoscopy, thereby reducing patient burden and complications. The development of esophageal varices is mainly associated with the left gastric vein (LGV). A previous study reported that the fractional flow change in the PV obtained with 4D flow MRI can predict the risk of esophageal varices bleeding2. In their study, the fractional flow change in the PV was used as an alternative method to the LGV because the LGV was too small to be visualized. We hypothesized that 4D flow MRI with low-velocity encoding sensitivity could provide direct estimation of the LGV. This study aimed to determine whether 4D flow MRI with low-velocity encoding sensitivity can predict the development of esophageal varices and stratify variceal bleeding risks.METHODS
Twenty-eight patients with chronic liver disease who underwent liver MRI and endoscopy at our institution were included in this study. 4D flow MRI was performed with a 3-T scanner using a 32-channel phased-array coil (anterior and posterior coil; Ingenia Elition 3.0T or Ingenia 3.0T CX Quasar Dual; Philips Healthcare, Best, Netherlands) under fasting and free-breathing conditions. MRI parameters were as follows: FOV, 400 mm; TR/TE, 5.3/3.7 ms; acceleration factor, 3.5; flip angle, 10°; acquisition matrix 1.67 x 2.45 x 4 mm, reconstruction matrix 0.83 x 0.83 x 2.00 mm, velocity encoding sensitivity 20 cm/s. The net flow volume (L/min) in the LGV, portal trunk, splenic (SPV), superior mesenteric (SMV), and azygos (AZV) veins was calculated using iTFlow2 (Cardio Flow Design). The fractional flow change in the PV was calculated using the following equation: [PV − (SMV + SPV)]/(SMV + SPV). The risk of esophageal varices was divided into three groups based on endoscopy findings:1) no varices group (no varices), 2) low-risk varices group (small varices and red color sign [RC sign] negative), and 3) high-risk varices group (F2 or higher or RC sign positive). The Spearman's rank correlation coefficient was used to assess a tendency toward the risk of variceal bleeding. In addition, receiver operating characteristic curve (ROC) analysis was performed to assess the diagnostic performance between the no varices and the varices groups (low-risk and high-risk varices groups), and between the high-risk varices and the other groups (no varices and low-risk varices groups).RESULTS
The risk of variceal bleeding was negatively and positively correlated with LGV and AZV, respectively (Figure 1). The net flow volume in the LGV showed the highest area under the curve (AUC) at 1.00 (95% Confidence interval (CI):0.88, 1.00) with a sensitivity of 100% and specificity of 100% (cut-off, ≤-0.007 L/min), followed by AZV at 0.90 (95% CI:0.73, 0.98), and fraction flow change in PV at 0.72 (95% CI:0.52, 0.87) between the no varices and varices groups. (Table 1). For differentiating the high-risk varices from the other groups, the AUC was highest in the AZV at 0.97 (95% CI:0.82, 1.00) with a sensitivity of 100% and specificity of 95.7% (cut-off, >0.131 L/min), followed by the LGV at 0.87 (95% CI:0.69, 0.97) and the splenic vein at 0.76 (95% CI:0.56, 0.90) (Table 2).DISCUSSION
LGV was directly evaluated using 4D flow MRI with low-velocity encoding sensitivity. The development of esophageal varices was associated with decreased and increased net flow volumes in the LGV and AZV, respectively. These results are theoretical, as LGV regurgitation is a major cause of esophageal varices and AZV is the drainage channel for esophageal varices. A decrease in fractional flow change in the PV was associated with the presence of esophageal varices but not with the risk of variceal bleeding. These results can be explained by the fact that the fractional flow change in the PV does not consider anatomic variations (e.g., the LGV drains into the splenic vein or splenic vein reflux), which may affect the diagnostic performance in identifying high-risk varices. Fractional flow change in the PV was used, despite its low AUC, when the LGV could not be directly visualized. Increased flow volume in the splenic vein was also associated with a risk of variceal bleeding. The elucidation of the reasons is challenging. Presently, we can only speculate that the increased flow volume in the SPV may be attributable to the hyperdynamic syndrome. Our results suggest that a cut-off value of 0.007 L/min for left gastric venous blood flow might help to avoid unnecessarily repeated endoscopy, and a cut-off value of 0.131 L/min for AZV could be used to decide whether endoscopic therapy should be performed.CONCLUSION
Direct flow measurement of the LGV with 4D flow MRI is a non-invasive quantitative biomarker for predicting the development of esophageal varices and stratifying bleeding risk.Acknowledgements
No acknowledgement found.References
1. Thekla H. Oechtering, Grant S. Roberts, et al. Clinical Applications of 4D Flow MRI in the Portal Venous System. Magn Reson Med Sci. 2022;21:340-353.
2. Motosugi U, Roldán-Alzate A, Bannas P, et al. Four-dimensional flow MRI as a marker for risk stratification of gastroesophageal varices in patients with liver cirrhosis. Radiology. 2019;290:101–7.
Figures
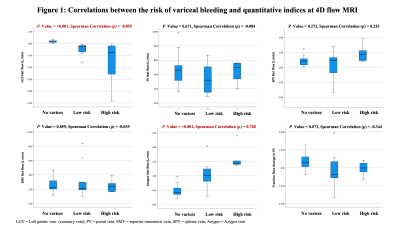
Figure 1: Correlations between the risk of variceal bleeding and quantitative indices at 4D flow MRI
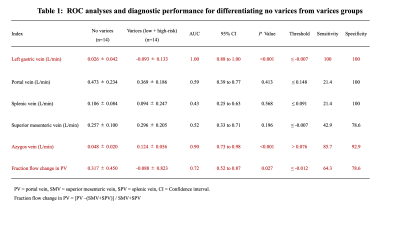
Table 1: ROC analyses and diagnostic performance for differentiating no varices from varices groups
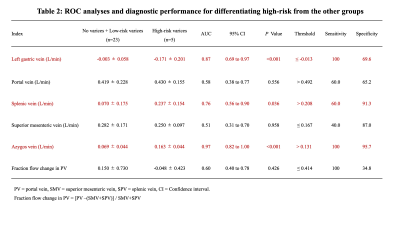
Table 2: ROC analyses and diagnostic performance for differentiating high-risk group from the other groups
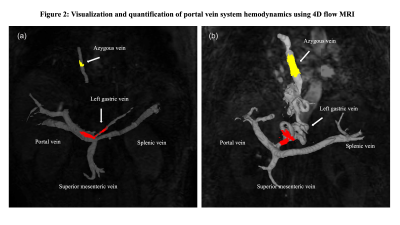
Figure 2: Visualization and quantification of portal vein system hemodynamics using 4D flow MRI. (a) The 4D flow MRI for a 78-year-old woman without esophageal varices shows hepatopetal flow of 0.024 L/min in the left gastric vein flowing into the portal vein and less flow of 0.035 L/min in the azygos vein. (b) The 4D flow MRI for a 76-year-old woman with high-risk varices shows a hepatofugal flow of -0.258 L/min in the left gastric vein and massive flow of 0.305 L/min in the azygos vein.
DOI: https://doi.org/10.58530/2023/2037