1997
Changes in the position of the eyeball in TAO patients with unilateral upper eyelid retraction by T2-weighted SPIR imaging1Department of Radiology, Peking University People’s Hospital, Beijing, China, 2Department of Ophthalmology, Peking University Third Hospital, Beijing, China, 3Department of Endocrinology, Peking University People’s Hospital, Beijing, China, 4Philips Healthcare, Beijing, China
Synopsis
Keywords: Image Reconstruction, Software Tools
For patients with thyroid-associated orbitopathy (TAO) presenting unilateral upper eyelid retraction, the phenomenon that the impaired eye is lower than the healthy eye (“eyeball descending”) has been noticed. This study investigated the eyeballs' position changes by 3D reconstitution of magnetic resonance (MR) images. With reference to the central plane of the healthy side, 70.37% impaired eyeballs (19/27) were found in significantly lower positions, and with significant positive correlations of increased thicknesses of levator palpebrae superioris (LPS), superior rectus (SR), and LPS-SR complex volume. This study provided objective evidence of “eyeball descending” in unilateral upper eyelid retraction TAO patients.Introduction
Thyroid-associated orbitopathy (TAO), known as Graves’ ophthalmopathy, is an autoimmune disease that impairs appearance and vision. Upper eyelid retraction is one of the most common clinical features of TAO1. In clinical practice, the phenomenon has been observed that the impaired eyeball’s position is lower than the healthy one among TAO patients with unilateral upper eyelid retraction (Figure 1). There were three presumptions to explain the phenomenon: 1)visual deviation due to increased margin reflex distance (MRD) or 2) eyeball rotation2; and 3) eyeball in a real lower position. The purpose of this study was to investigate the position changes of eyeballs in TAO patients presenting unilateral upper eyelid retraction by 3D reconstitution of magnetic resonance (MR) images, which may provide an objective evidence for treatment decision-making.Methods
Twenty-seven TAO patients (Average age,34.81 ± 9.802 years; range, 20-58 years; five males, twenty-two females) , with the only clinical presentation of unilateral upper eyelid retraction were included in this study. Moreover, the difference of proptosis wasn't more than 1mm in each patient. Standardized orbital MR were performed by 3.0T system (Ingenia, Philips Healthcare, the Netherlands). The following shows the post-processing process on 3D slicer software (version 5.0.3): Firstly, on coronal T2-weighted SPIR orbital images, the direction and distance of the eyeball’s horizontal plane of the impaired side from the healthy eyeball’s reference plane were measured, as well as the thickness of the levator palpebrae superioris (LPS) muscle and superior rectus (SR) muscle (Figure 3A). Secondly, 3D images were reconstructed from coronal T2-weighted SPIR MR imaging and then measured direction and angle of eyeball’s rotation compared to healthy eye (Figure 3B). Thirdly, LPS-SR complex volume were calculated at reconstructed oblique sagittal MR images. Statistical analyses were performed using IBM SPSS Statistics (SPSS version 29.0). One sample Wilcoxon test and Mann–Whitney U test was used to analyze the quantitative data. Correlation between these variables was performed by using the spearman correlation.Results
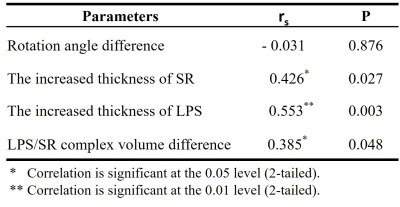
In this study, eyeballs of 70.37% patients (19/27) were in a lower position, with reference to the central plane of the healthy eyes. The mean descending distance of 27 patients was 0.97 ± 1.73mm (p = 0.008).All 27 patients had a thicker SR on the impaired side (6.97 ± 2.52mm vs. 4.23 ± 0.93mm, p<0.001). Moreover, 96.30%(26 / 27 )patients presented with LPS hypertropia on the impaired side ( 4.73 ± 1.36mm vs 3.29 ± 1.08mm, p < 0.001). There was a significant positive correlation between descent distance in the impaired eyes and increased thickness of LPS (R= 0.553, p = 0.003). Moreover, the descent distance was also correlated with increased thickness of SR (R= 0.426, p = 0.027) and increased LPS/SR complex volume (R = 0.385, p = 0.048). However, there was no significant correlation between the descent distance and the rotation angle of the impaired eye (R= -0.031, p = 0.876). According to the rotation direction of the impaired eyeball on reconstructed oblique sagittal MR images, patients were divided into two groups: the down-rotation and the up-rotation groups. In the down-rotation group, the rotation angle had a significant correlation with the increased thickness of SR (R = 0.698, p = 0.008). In the up-rotation group, the rotation angle had significant correlation with descent distance (R = 0.593, p = 0.026) and the increased thickness of LPS (R = -0.575, p = 0.032) (Figure 4).Discussion
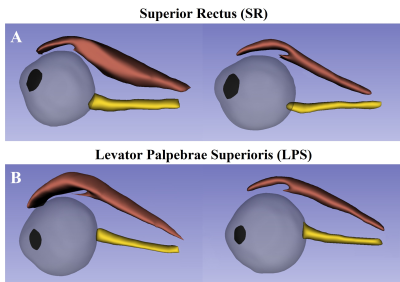
In this study, the impaired eyeball of descended compared to that of the healthy eye in 70.37% of twenty-seven TAO patients with unilateral upper eyelid retraction. Moreover, the descent distance was positively correlated with the increased thickness of LPS, SR, and LPS-SR complex volume. It was confirmed increased LPS-SR complex volume was associated with unilateral upper eyelid retraction in TAO patients2. It indicated the eyeballs’ descending was associated with pathological changes of LPS and SR, not a pure visual deviation. SR and LPS are referred to as the LPS-SR complex. However, due to the different positions of the muscle belly, they could be distinguished when their incrassation is caused by TAO. Therefore, the thicknesses of the SR and LPS were measured separately in this study. Compared with the thickened SR, the thickened LPS has a greater correlation with the eyeballs’ descending. A possible explanation is the different positions between the thickened LPS and SR (Figure 5). It's also observed the rotation angle was correlated with the increased thickness of SR muscle in the down-rotation group. Furthermore, the increased thickness of LPS had a negative correlation with the rotation angle in the up-rotation group, but the increased thickness of SR didn’t show a significant correlation. It’s likely to be related to restrictions from the thickened LPS or SR. A previous study found because of the restriction from an enlarged LPS/SR complex, the majority of TAO patients with LPS/SR complex hypertropia suffered from ipsilateral vertical strabismus3. Meantime, that means the phenomenon of eyeball descending on clinical pictures could partially be caused by virtual deviation, especially in patients with SR prominent enlargement.Conclusions
Eyeball’s descending of the eyeball in TAO patients with unilateral upper eyelid retraction was associated with pathological changes of LPS and SR, rather than a pure visual deviation.Acknowledgements
No acknowledgement.References
1. Bahn, R. S. Graves’ ophthalmopathy. N Engl J Med 362, 726–738 (2010).
2. Byun, J. S. & Lee, J. K. Relationships between eyelid position and levator-superior rectus complex and inferior rectus muscle in patients with Graves’ orbitopathy with unilateral upper eyelid retraction. Graefes Arch Clin Exp Ophthalmol 256, 2001–2008 (2018).
3. Wang, Y. et al. Thyroid eye disease presenting with superior rectus/levator complex enlargement. Orbit 39, 5–12 (2020).
Figures
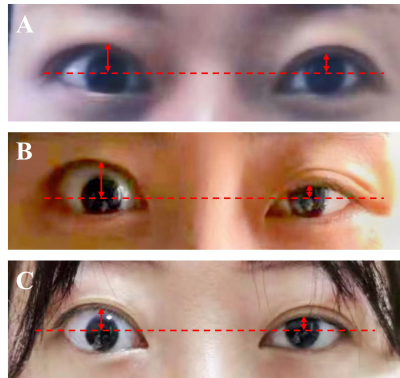
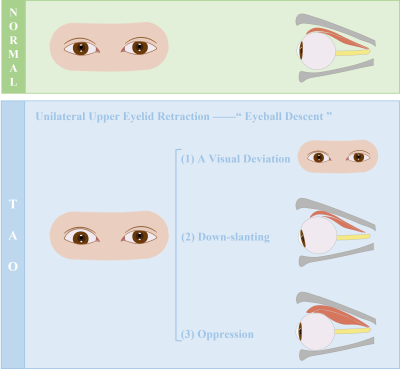
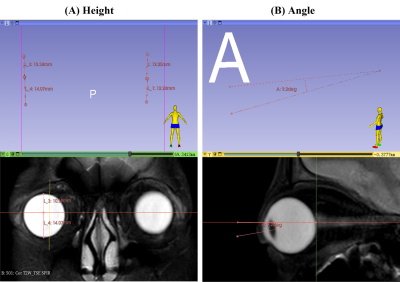
Figure 3:There was a TAO patient with right upper eyelid retraction. (A) The center plane of the healthy eyeball was used as the reference plane. The distance of the eyeball’s horizontal plane of the impaired side from the reference plane were measured and recorded in coronal T2-weighted SPIR orbital images by 3D slicer software. (B)3D images were reconstructed from coronal T2-weighted SPIR MR imaging by 3D slicer software and then measured direction and angle of eyeball’s rotation.