1992
Cost Analysis of Cardiac MRI for Cardiac Transplant Surveillance1Pediatrics, Medical College of Wisconsin/ Herma Heart Institute at Children's Wisconsin, Milwaukee, WI, United States, 2Pediatrics, Medical College of Wisconsin, Milwaukee, WI, United States, 3Pediatrics, Vanderbilt University Medical Center, Nashville, TN, United States, 4Grainger College of Engineering, Carle Foundation Hospital/University of Illinois, Urbana, IL, United States, 5Pediatrics, Vanderbilt Univesity Medical Center, Nashville, TN, United States, 6University of Notre Dame Mendoza College of Business, Notre Dame, IN, United States
Synopsis
Keywords: Cardiovascular, Health Care Economics, Heart Transplantation; Acute Rejection
Current transplant surveillance relies on frequent cardiac catheterization with endomyocardial biopsy (cath EMB) to detect life threatening acute rejection. Cardiac MRI has emerged as a diagnostic tool which can characterize the myocardium. The PEACE study (R01-HL164995-01) aims to evaluate the potential for using cardiac MRI parametric mapping as a pre-cath EMB screening tool to alleviate both patient and family burden and the financial burden of cath EMB. Consistent with the recent emphasis on "Value MRI," we therefore sought to understand the potential Medicare savings, if MRI is used for transplant surveillance for healthy heart transplant recipients rather than cath EMB.Introduction
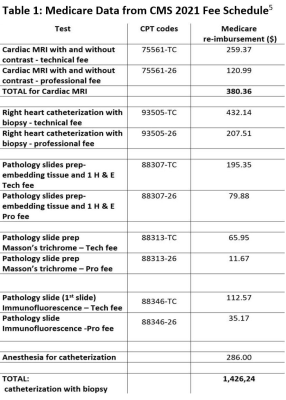
National health expenditures in the United States, expressed as percent of gross domestic product (GDP), have risen steadily from 1960 to 2020.1 As new medical technologies have offered improvements in healthcare outcomes, costs have risen and are now at ~19% of GDP. While lifesaving therapies exist for many acquired and congenital heart diseases, heart transplantation may become necessary. In 2020, a heart transplant cost an average of $1,664,800 – an amount which includes pre and post-transplant medical care, organ procurement, hospital charges, medications, and physician fees.2 Worldwide, over 6000 heart transplants are performed annually, with over 700 for recipients who are less than 18 years old.3,4 Current transplant surveillance relies on frequent cardiac catheterization with endomyocardial biopsy (cath EMB) to detect life threatening acute rejection. For the pediatric population, this procedure requires anesthesia – adding risk and cost. Cardiac MRI has emerged as a useful diagnostic tool which can characterize the myocardium by identifying myocardial edema, myocardial fibrosis, and scar. Increasingly, this modality is being employed for transplant patients, and the PEACE study (R01-HL164995-01) aims to evaluate the potential for using cardiac MRI parametric mapping as a pre-cath EMB screening tool that would alleviate both patient and family burden and the financial burden of cath EMB (Table 1).5 Consistent with the recent emphasis on "Value MRI," we therefore sought to understand the potential Medicare savings, if MRI is used for transplant surveillance for healthy heart transplant recipients rather than cath EMB, at several levels of positive test rate for cardiac MRI.Methods
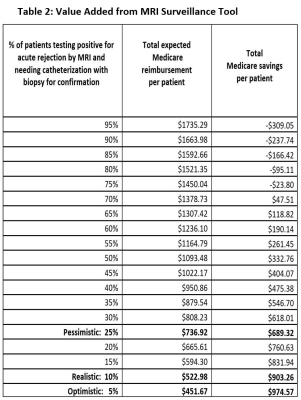
With an annual acute rejection incidence of 2.5 – 5% on surveillance cath EMB6, case scenarios were modeled with focus on the realistic, pessimistic, and optimistic positive test rate of surveillance MRI using parametric T1 and T2 mapping. In all scenarios, we assume a negative predictive value of >/= 95%, which is comparable to both our preliminary data and the negative predictive value of cell-free DNA. Because cath EMB is the current "gold standard" for detecting acute rejection, if surveillance MRI shows features consistent with acute rejection (elevated T2, elevated extracellular volume)7,8, cath EMB will provide confirmation; therefore, the financial burden includes both tests ($380.36 + 1426.24 = $1806.60). If surveillance MRI shows negative results, then no cath EMB is performed, and the cost will be only $380.36 for MRI. Using probability theory, the "expected value" per patient was calculated by:Cost/patient = $1806.60*PCMR + $380.36*NCMR with PCMR the positive rate for cardiac MRI and NCMR the negative rate.
The difference between $1426.24 (cath only) and this "expected value" of MRI surveillance with confirmatory cath, gives the total Medicare savings per patient.
$1426.24 – ($1806.60*PCMR + $380.36*NCMR) = Medicare savings
Results
Table 2 shows the total Medicare cost per patient-test and the Medicare cost savings per patient-test across a full range of putative positive test rates for cardiac MRI; highlighted in bold text are the realistic, pessimistic, and optimistic scenarios. In the realistic scenario, MRI would result in 10% of patients being positive; this assumes a positive predictive value of 50%, with half of those with positive MRI actually having a positive biopsy. The Medicare reimbursement would be 1806.60*0.1+380.36*0.9=522.98. In this situation, savings would be an average of $903.26 per patient. In the pessimistic case, MRI suggests rejection 25% of the time, requiring more catheterization to detect the true positive MRI cases. While Medicare reimbursements would be higher as additional catheterizations are performed, Medicare cost savings are nonetheless present, because only 25% of patients require cath EMB rather than all subjects. This situation represents is a comparable rate of rejection detection as afforded by donor fraction cell-free DNA.9,10 With this rate of positive MRI test, 80% will ultimately be false positive based on cath EMB, but this still results in a Medicare cost savings of $689.32 per patient. Optimistically, MRI would only detect rejection in 5% - all confirmed by cath EMB. In this situation, the positive predictive value would be 100%, and the cost savings would be $974.57 per patient.Discussion
At even the most pessimistic positive predictive values considered, these modeling results suggest substantial Medicare cost savings for using cardiac MRI parametric mapping as a screening tool for acute cardiac rejection. While modeled using Medicare data, the financials are notably higher for commercial payors (3 - 10 times the Medicare rate depending on CPT code). Over the lifetime of a heart transplant recipient, financial savings afforded by surveillance cardiac MRI, rather than initial surveillance cath EMB, would be substantial given the testing frequency (six plus times in the first year and annually thereafter at most centers) and expense of cath EMB. False negative MRI testing cannot be modeled here, though the goal in creating a screening test would be to optimize the negative predictive value at the expense of the positive predictive value. This modeling approach also does not account for the savings to patients’ and patient families’ personal costs, such as lost work time, transportation, and other expenses associated with the more extensive cath EMB procedure.Acknowledgements
No acknowledgement found.References
1. https://www.statista.com/statistics/184968/us-health-expenditure-as-percent-of-gdp-since-1960/
2. https://www.medicalnewstoday.com/articles/heart-transplant-cost#cost
3. Khush KK, Cherikh WS, Chambers DC, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-fifth Adult Heart Transplantation Report-2018; Focus Theme: Multiorgan Transplantation. J Heart Lung Transplant 2018; 37:1155-68.
4. Rossano JW, Cherikh WS, Chambers DC, et al. The Registry of the International Society for Heart and Lung Transplantation: Twentieth Pediatric Heart Transplantation Report-2017; Focus Theme: Allograft ischemic time. J Heart Lung Transplant 2017; 36:1060-9.
5. http://www.cms.gov/medicare/physician-fee-schedule/search
6. Peng DM, Ding VY, Hollander SA, et al. Long-term surveillance biopsy: Is it necessary after pediatric heart transplant? Pediatr Transplant 2019 Feb;23(1): e13330.
7. Imran M, Wang L, McCrohon J, et al. Native T1 Mapping in the Diagnosis of Cardiac Allograft Rejection: A Prospective Histologically Validated Study JACC Cardiovasc Imaging 2019;12:1618-28
8. Vermes E, Pantaléon C, Auvet A, et al. Cardiovascular magnetic resonance in heart transplant patients: diagnostic value of quantitative tissue markers: T2 mapping and extracellular volume fraction, for acute rejection diagnosis. J Cardiovasc Magn Reson 2018; 20:59
9. Richmond ME, Zangwill SD, Kindel SJ, et al. Donor fraction cell-free DNA and rejection in adult and pediatric heart transplantation. J Heart Lung Transplant 2020 May;39(5):454-463.
10. Richmond ME, Deshpande SR, Zangwill SD et al. Validation of donor fraction cell-free DNA with biopsy-proven cardiac allograft rejection in children and adults. J Thorac Cardiovasc Surg2022 Apr 30; S0022-5223(22)00508-6.