1984
Comprehensive 4D flow MRI analysis of aortic flow hemodynamics in pediatric/young adult patients with bicuspid aortic valve1Department of Radiology, Children's Hospital Colorado, University of Colorado Anschutz Medical Campus, Aurora, CO, United States, 2Department of Radiology, Northwestern University, Chicago, IL, United States, 3Department of Pediatrics, University of Colorado Anschutz Medical Campus, Children’s Hospital Colorado, Aurora, CO, United States, 4Department of Bioengineering, University of Colorado Anschutz Medical Campus, Aurora, CO, United States
Synopsis
Keywords: Flow, Velocity & Flow, 4D flow MRI
Bicuspid aortic valve is associated with progressive aortic dilatation, which is seen both in pediatric and adult populations. Although several studies have found a connection between aortic hemodynamics, vessel wall architectural abnormalities, and progressive dilation, the role of hemodynamics in pediatric aortopathy remains unclear. We used 4D flow MRI data in pediatric bicuspid aortic valve patients to identify potential hemodynamic biomarkers associated with aortic diameter. Despite no clear association with aortic diameter, different flow features between BAV patients with/without coarctation were found.Introduction
Bicuspid aortic valve (BAV) is one of the most common congenital heart defects with a prevalence of 1-2%1. The aorta of BAV patients is more likely to be dilated compared to the general population, with monitoring and surgical guidelines predicated on the risk for aortic aneurysm and dissection. Routine monitoring for progression of aortic dilation is recommended by consensus guidelines, but no evidence or predictors have been identified in children to predict aortic dilatation or assess risk for dissection. 4D flow MRI (time-resolved, three-dimensional phase-contrast MRI) is a promising tool for risk stratification in pediatric patients with BAV. Several 4D flow studies in adult BAV patients have shown unique hemodynamic characteristics predictive of growth or abnormal tissue biomechanics2. Wall shear stress (WSS) is one such blood flow feature, as its close association with elastic fiber degradation in the aorta was recently reported3. Although progressive aneurysms are also observed in pediatric BAV patients4, 4D flow investigations in young patients are limited and possibly etiologically different compared to adults5,6. In prior studies, WSS has not been conclusively predictive of aortic dilatation, possibly due to small sample sizes. Another challenge in pediatric BAV study is a wide variety of comorbidities, such as aortic coarctation, which may result in variability in obtained hemodynamic quantities. Here, we conduct a retrospective 4D flow analysis in pediatric/young adult BAV patients to investigate if there are hemodynamic indicators of aortic dilatation. We hypothesize that hemodynamic biomarkers will correlate with aortic diameter (aortic Z-score) and comorbidities seen in BAV patients affect hemodynamics in the aorta.Methods
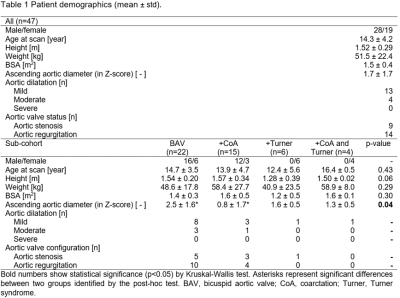
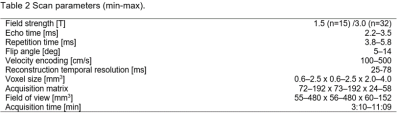
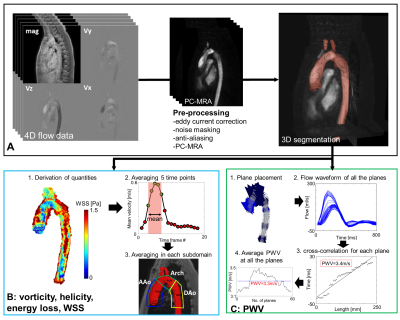
This IRB-approved retrospectively study investigated 47 BAV patients who underwent cardiac 4D flow MRI and were less than 20 years old at the time of scan from our hospital database (mean age, 14.3 ± 4.2 years; Table 1). Patients were scanned with Philips Ingenia (Philips Healthcare, Best, Netherlands; scan parameters in Table 2). Patients were divided into 4 subgroups: BAV, BAV with aortic coarctation, BAV with Turner syndrome, and BAV with both aortic coarctation and Turner syndrome. The 4D flow MRI analysis and methods of these patients are illustrated in Fig. 1. 4D flow MRI post-processing was performed to correct eddy currents, mask noise, anti-alias velocity, and to create phase-contrast MR angiography (PC-MRA) images using custom MATLAB scripts7. Based on the PC-MRA, the aorta was segmented automatically using a deep learning framework,8,9 followed by manual correction. WSS, helicity, vorticity, and viscous energy loss were computed using previously described approaches10,11. Here, 5 temporal phases centered at peak flow systole were averaged to obtain the peak-systolic quantities and the obtained values were further averaged for three subdomains: ascending aorta (AAo), aortic arch, and descending aorta. Aortic pulse wave velocity was also obtained by cross-correlation approach12. Pearson correlation between the obtained hemodynamic metrics and AAo Z-score, as obtained from medical records, were evaluated. Subgroup comparison for hemodynamic quantities excluded two subgroups (BAV with Turner syndrome, n=6; BAV with both aortic coarctation and Turner syndrome, n=4) due to the small number of subjects. A Kruskal-Wallis test and post-hoc analysis with Bonferroni correction were employed for more than three group comparison with p=0.05 as a significance level, while an Wilcoxon rank sum test was used for two group comparisons.Results
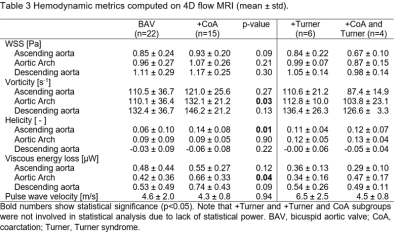
The BAV subgroup showed larger AAo Z-score than those with coarctation (2.5 ± 1.6 in BAV vs. 0.8 ± 1.7 in BAV with coarctation, p=0.03; Table 1). For the entire cohort (N=47), no significant correlation was found between AAo Z-score and hemodynamic quantities at the AAo (R=-0.25-0.13, p=0.09-0.84; Fig.2A-E). Overall, no strong correlation was found between Z-score and the obtained quantities (Fig.2F). Comparison between BAV and coarctation subgroups found significant differences in vorticity in the aortic arch (p=0.03), helicity in the AAo (p=0.01), and viscous energy loss in the aortic arch (p=0.04) (Table 3). Correlation analysis in each subgroups showed different tendency (Fig.2G,H).Discussion
Correlation analysis did not find a strong hemodynamic association with aortic Z-score, contrary to our hypothesis. The lack of correlation between pulse wave velocity and AAo diameter suggests inherent aortic wall property may not be a dominant factor for progressive aortic dilatation in early stage of life; however, more study is needed given the limited temporal resolution of 4D flow MRI. The results agree with a previous study in adults, reporting altered wall stiffness is seen at older age, rather than adolescence13. On the other hand, lesion-specific hemodynamic features were found; BAV patients with coarctation had larger vorticity and viscous energy loss at the aortic arch, and larger helicity at the AAo than those without coarctation. A previous study found altered hemodynamics (WSS, peak velocity) at the arch and descending aorta in BAV patients with coarctation5. Our study implies altered hemodynamics can also be seen for the proximal aorta. Although significantly different AAo Z-score confound these results, it suggests BAV combined with coarctation may produce unique flow features.Conclusion
A clear association between aortic Z-score and hemodynamic quantities were not found in this study while lesion-specific flow features were found for the proximal aorta. Considering large variability in comorbidity and lesion-specific hemodynamic differences of these pediatric patients, proper subgroup analysis, larger study sizes and longitudinal monitoring is necessary.Acknowledgements
NIH R01HL133504 (AJB)
NIH NIA P30AG059988 (KJ)
References
1. Ward C. Clinical significance of the bicuspid aortic valve. Heart. 2000;83:81-85.
2. Barker AJ, Markl M, Burk J, Lorenz R, Bovk J, Bauer S, Schulz-Menger J, von Knobelsdorff-Brenkenhoff F. Bicuspid aortic valve is associated with altered wall shear stress in the ascending aorta. Circ Cardiovasc Imag. 2012;5:457-466. doi:10.1161/CIRCIMAGING.112.973370.
3. Guzzardi DG, Barker AJ, van Ooij P, Malaisrie SC, Puthumana JJ, Belke DD, Mewhort HEM, Svystonyuk DA, KangS, Verma S, Collins J, Carr J, Bonow RO, Markl M, Thomas JD, McCarthy PM, Fedak PWM. Valve-related hemodynamics mediate human bicuspid aortopathy; insight from wall shear stress mapping. J Am Coll Cardiol. 2015;66:2112-2120 e2. doi:10.1016/j.jtcvs.2018.05.095.
4. Warren AE, Boyd ML, O’Connell, Dodds L. Dilatation of the ascending aorta in paediatric patients with bicuspid aortic valve: frequency, rate of progression and risk factors. Heart. 2006;92:1496-1500. doi: 10.1136/hrt.2005.081539
5. Allen BD, van Ooij P, Barker AJ, Carr M, Gabbour M, Schnell S, Jarvis KB, Carr JC, Markl M, Rigsby C, Robinson JD. Thoracic aorta 3D hemodynamics in pediatric and young adult patients with bicuspid aortic valve. J Magn Reson Imaging. 2015;42:954-963.
6. Rose MJ, Rigsby CK, Berhane H, Bollache E, Jarvis K, Barker AJ, Schnell S, Allen BD, Robinson JD, Markl M. 4-D flow MRI aortic 3-D hemodynamics and wallshear stress remain stable over short-term follow-up in pediatric and young adult patients with bicuspid aortic valve. Pediatr Radiol. 2019;49:57-67.
7. Bock J, Kreher B, Hennig J, Markl M. Optimized pre-processing of time-resolved 2D and 3D phase contrast MRI data. Proceedings of International Society for Magnetic Resonance in Medicine. 2007;15:3138
8. Fujiwara T, Berhane H, Scott MB, Englund EK, Schafer M, Fonseca B, Berthusen A, Robinson JD, Rigsby CK, Browne LP, Markl M, Barker AJ. Segmentation of the Aorta and Pulmonary Arteries Based on 4D Flow MRI in the Pediatric Setting Using Fully Automated Multi-Site, Multi-Vendor, and Multi-Label Dense U-Net. J Magn Reson Imag 2022;55:1666-1680. doi: 10.1002/jmri.27995.
9. Berhane H, Scott M, Elbaz M, Jarvis K, McCarthy P, Carr J, Malaisrie C, Avery R, Barker AJ, Robinson JD, Rigsby CK, Markl M. Fully automated 3D aortic segmentation of 4D flow MRI for hemodynamic analysis using deep learning. Magn Reson Med. 2020;84:2204-2218.
10. van Ooij P, Potters WV, Nederveen AJ, Allen BD, Collins J, Carr J, Malaisrie SC, Markl M, Barker AJ. A methodology to detect abnormal relative wall shear stress on the full surface of the thoracic aorta using four-dimensional flow MRI. Magn Reason Med. 2015;73(3):1216-1227. doi.org/10.1002/mrm.25224.
11. Fujiwara T, O’Callaghan B, Shafer M, DiMaria M, Fonseca B, Barker AJ. Investigation of Aortic Wall Thickness, Stiffness and Flow Reversal in Patients With Cryptogenic Stroke: A 4D Flow MRI Study. SCMR 24th Annual Scientific Sessions. 2021 (Virtual).
12. Jarvis K, Soulat G, Scott M, Vali A, Pathrose A, Syed AA, Kinno M, Prabhakaran S, Collins JD, Markl M. Investigation of Aortic Wall Thickness, Stiffness and Flow Reversal in Patients With Cryptogenic Stroke: A 4D Flow MRI Study. J Magn Reson Imag. 2020;53:942-952.
13. Johnson EM, Scott MB, Jarvis K, Allen BD, Malaiserie SC, McCarthy P, Fedak P, Barker AJ, Markl M. Association of bicuspid aortopathy with global aortic stiffness: a 4D flow MRI study in 584 subjects. SCMR 24th Annual Scientific Sessions. 2021 (Virtual).
Figures