1983
Novel non-invasive cardiac MR oximetry and 4-dimensional flow in single ventricle hearts1Lurie Children's Hospital/Northwestern University Feinberg School of Medicine, Chicago, IL, United States, 2Northwestern University, Chicago, IL, United States, 3Ohio State University, Columbus, OH, United States
Synopsis
Keywords: Cardiovascular, Translational Studies, 4D Flow
Cardiac magnetic resonance imaging can provide novel non-invasive estimation of blood oxygen saturation and quantification of blood flow streaming in pediatric and adult patients with complex single ventricle physiology. Non-uniform distribution of inferior and superior caval blood flow and oxygenation to the left and right lungs may cause complications in patients with Fontan circulation. An individualized, comprehensive approach may identify patients at risk.Introduction
Non-invasive evaluation of blood oxygen saturations (oximetry) and flow distribution by cardiac MR has clinical application in single ventricle physiology – the most complex form of congenital heart disease. Single ventricle patients undergo staged palliative approaches typically ending with the Fontan circulation. Despite increased survival, many patients develop “failing Fontan physiology” while others are largely morbidity-free1-2. Initial clinical presentations include exercise intolerance and unexplained cyanosis. A feature of failing circulation is the abnormal course and extent of deoxygenated blood streaming3-4. The low-pressure Fontan system is particularly susceptible to small alterations in streaming. This study is the first attempt to evaluate the relationship between oxygenation and flow distribution in these patients by combining our previously validated oximetry MRI protocol in children and adults with congenital heart disease with 4D flow MRI5-6.Methods
4 patients with single ventricle physiology (ages in years: 14, 15, 12, 32; 1 female) undergoing clinically indicated cardiac MRI, including 4D flow MRI, were recruited in a single tertiary care children’s hospital. For oximetry in each patient, a series of T2-prepared single-shot steady-state free-precession images were acquired in free-breathing, across T2-preparation times of 0 to 200 ms (Figure 1). Images were acquired in planes to evaluate the inferior and superior caval veins and pulmonary arteries. Color coded maps representing estimated oxygen saturations were created based on voxel-wise fitting of the T2 data to the Luz-Meiboom model (S , T , τ , and α). 4D flow analysis included the placement of 2D analysis planes at the inferior and superior caval veins and right and left pulmonary arteries to quantify absolute blood flow in each vessel and percentage of flow to each lung (Figure 1).Results
Schematics for each patient show oxygen saturations and absolute blood flow in the caval veins and pulmonary arteries as well as percentage of blood flow from each caval vein to each pulmonary artery (Figures 2-5). In patient 1 (14-year-old female, extracardiac fenestrated Fontan) and patient 2 (15-year-old male, lateral tunnel Fontan), both caval veins preferentially stream blood flow to the right pulmonary artery with minimal change to the oxygen saturation (Figures 2,3). There is an increase in oxygen saturation to the left pulmonary artery. This is possibly due to multiple small collateral vessels seen in patient 1 and contribution from a left superior caval vein in patient 2. Patient 3 (12-year-old male, extracardiac Fontan without fenestration) has preferential inferior vena cava/Fontan flow streaming to the right pulmonary artery and superior vena cava flow streaming to the left pulmonary artery with corresponding oxygen saturations (Figure 4). Patient 4 (32-year-old male, lateral tunnel Fontan) has similar streaming patterns compared to patient 3 but with an opposite saturation differential between the pulmonary arteries (Figure 5). This is potentially due to his extensive network of observed aortopulmonary collateral vessels (collateral percentage calculated as 43%). He presented clinically with increasing systemic cyanosis.Discussion
This case study demonstrates feasibility of our combined oximetry and 4D flow approach for non-invasive evaluation of the relationship between oxygen saturations and blood flow streaming in complex congenital heart disease. During invasive catheterization (current gold standard), point blood gas samples from select cardiac chambers and vessels are obtained and extrapolated to estimate oxygen saturations in the remaining heart and vasculature based on presumed hemodynamics while ignoring streaming effects. Each patient in this study had unique streaming patterns of deoxygenated blood flow suggesting that comprehensive individualized evaluation may be warranted in complex patients to understand their clinical complications and surveillance needs.Conclusion
Streaming effects should be considered when evaluating single ventricle patients, particularly those with “failing” physiology. Ongoing patient recruitment is warranted to further optimize MR image acquisition and analysis, enhance visualization of streaming effects of oxygenated and deoxygenated blood, and correlate data to clinical presentations.Acknowledgements
NoneReferences
1. Mellion K, Uzark K, Cassedy A, et al. Health-related quality of life outcomes in children and adolescents with congenital heart disease. J Pediatr. 2014;164(4):781-788.
2. Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019 Apr 2;73(12):1494-1563.
3. Rychik J, Atz AM, Celermajer DS, et al. Evaluation and management of the child and adult With Fontan circulation: A scientific statement from the American Heart Association. Circulation. 2019; 1.
4. Von Rhein M, Buchmann A, Hagmann C, et al. Brain volumes predict neurodevelopment in adolescents after surgery for congenital heart disease. Brain. 2014;137(1):268-276.
5. Varghese J, Smyke M, Pan Y, et al. Patient-adaptive magnetic resonance oximetry: comparison with invasive catheter measurement of blood oxygen saturation in patients with cardiovascular disease. J Magn Reson Imaging. 2020;52(5):1449-1459.
6. Jarvis K, Schnell S, Barker AJ, et al. Evaluation of blood flow distribution asymmetry and vascular geometry in patients with Fontan circulation using 4-D flow MRI. Pediatr Radiol. 2016;46(11):1507-19.
Figures
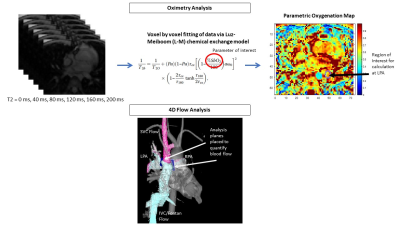
Figure 1. Method model (patient 1, 14-year-old female, extracardiac fenestrated Fontan). Top: Six single-shot steady-state free-precession images acquired free-breathing across T2-preparation times (0-200 ms). Color coded oximetry maps to estimate oxygen saturations were created via voxel-wise fitting of T2 data to the Luz-Meiboom model (S , T , τ , and α). Bottom: Analysis planes were placed at the superior vena cava (SVC), inferior vena cava (IVC), right pulmonary artery (RPA) and left pulmonary artery (LPA) to quantify absolute blood flow and depict preferential streaming.
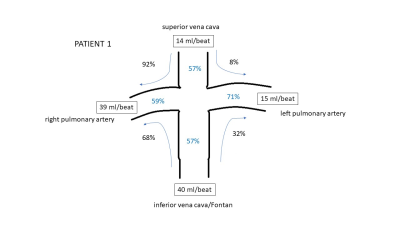
Figure 2. Schematic of Fontan circulation and flow distribution of caval veins to pulmonary arteries for patient 1, 14-year-old female with an extracardiac fenestrated Fontan. Oxygen saturations depicted in blue. Both caval veins preferentially stream blood flow to the right pulmonary artery with minimal change to the oxygen saturation. There is an increase in oxygen saturation in the left pulmonary artery - possibly explained by multiple small collateral vessels.
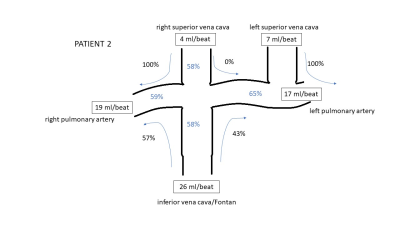
Figure 3. Schematic of Fontan circulation and flow distribution of caval veins to pulmonary arteries for patient 2, 15-year-old male with a lateral tunnel Fontan. Oxygen saturations depicted in blue. The right superior vena cava (SVC) streams blood flow entirely to the right pulmonary artery (RPA) and left SVC to the left pulmonary artery (LPA). The inferior vena cava/Fontan preferentially streams flow to the RPA with minimal change to oxygen saturation. There is increase in oxygen saturation in the LPA - possibly explained by contribution from the left SVC.
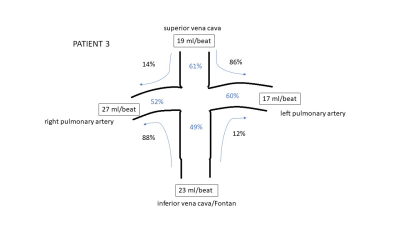
Figure 4. Schematic of Fontan circulation and flow distribution of caval veins to pulmonary arteries for patient 3, 12-year-old male with an extracardiac Fontan without fenestration. Oxygen saturations depicted in blue. The superior vena cava preferentially streams blood flow to the left pulmonary artery. The inferior vena cava/Fontan preferentially streams flow to the right pulmonary artery. Oxygen saturations correspond to the flow streaming pattern.
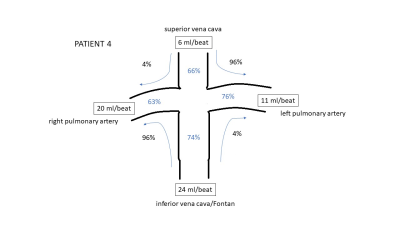
Figure 5. Schematic of Fontan circulation and flow distribution of caval veins to pulmonary arteries for patient 4, 32-year-old male with a lateral tunnel Fontan and increasing systemic cyanosis. Oxygen saturations depicted in blue. The superior vena cava preferentially streams blood flow to the left pulmonary artery. The inferior vena cava/Fontan preferentially streams flow to the right pulmonary artery. Oxygen saturations are opposite to the flow streaming pattern – possibly due to large aortopulmonary collateral network.