1978
The importance of cardiac MRI (CMR) in pediatric acute myocarditis, and it’s correlation with high sensitivity troponin1Pediatric Cardiology, UT Southwestern, Dallas, TX, United States, 2Pediatric Radiology, UT Southwestern, Dallas, TX, United States
Synopsis
Keywords: Cardiovascular, Myocardium, Myocarditis, LGE, troponin
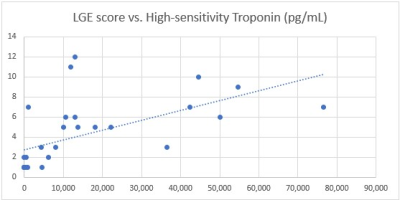
Pediatric myocarditis is associated with major morbidity and mortality. Biomarkers are needed to predict clinical outcomes. High-sensitivity troponin (hs-TnT) and late gadolinium enhancement (LGE) have been shown to correlate with poor outcomes in adult populations. We found that LGE and hs-TnT linearly correlated with each other in our pediatric population, and that children with myocarditis were more likely to be male, have a higher LGE score, higher hs-TnT values, and increased T2 signal intensity than those who did not. A cut-off of 1200 ms for native T1 global mean was significantly associated with the need for inotropic support.Introduction
Pediatric acute myocarditis is a major cause of morbidity in young patients. Adult studies have shown positive correlation between high sensitivity troponin (hs-TnT) and late gadolinium enhancement (LGE)1,2. We sought to assess correlation of this biomarker with LGE in pediatric patients with acute myocarditis, and its ability to predict clinical outcomes.Methods
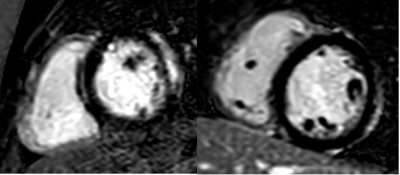
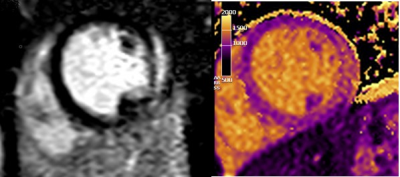
This was a retrospective observational study of consecutive patients undergoing CMR due to elevated hs-TnT for clinical reasons between 04/2021 to 10/2022. Patients were excluded if hs-TnT was not drawn or CMR was not obtained at the time of acute illness, if hs-TnT was not obtained within 3 months of CMR for subacute illness, or if LGE could not be assessed on CMR. LGE was described as typical (subepicardial), atypical, or none and given a quantitative score of 1-18 based on the amount of AHA segments involved3, with a modifier if LGE was >75% transmural (figure 1A & 1B). Patients underwent CMR on a 1.5-T system (Philips Healthcare, Best, The Netherlands). For image acquisition, patients were placed in supine position and images were acquired at repeat breath holds with ECG gating. CMR sequences routinely obtained included T2-weighted dark-blood fast-spin-echo (FSE) sequences and pre- and post-gadolinium T1-weighted FSE sequences using a modified-look-locker-inversion-recovery (MOLLI) 4-1-3-1-2s sequence, with single breath-hold inversion recovery measurements and subsequent T1 map reconstruction. Phase-sensitive inversion recovery (PSIR) spoiled gradient echo sequences were used for late-enhancement, and the inversion time was individually adjusted to null normal myocardium. If the patient’s clinical status was stable, 3-dimensional whole heart imaging using balanced steady-state free precession with respiratory navigation and electrocardiogram triggering in diastole was obtained to assess coronary anatomy.Results
A total of 45 patients were reviewed. 14 were excluded and 31 patients met inclusion criteria. 19 (61%) had viral myocarditis, including 2 (6%) with myocarditis attributed to COVID-19 vaccination, and 1 (3%) with acute coronavirus (non-COVID-19) myocarditis. Median age was 16.5 ± 4.8 years old, 25 (81%) patients were male, 4 (13%) required inotropic support, none required ECMO, or underwent heart transplant or died. There was a high correlation between hs-TnT and LGE score in the entire cohort (R2=0.6; p < 0.0005) (figure 2). Patients who had myocarditis all had a subepicardial (typical) pattern of LGE and exhibited higher hs-TnT values (23,004 ± 21,382 pg/mL vs 570 ± 1,255 pg/mL; p=0.001), higher LGE score (6 ± 3 vs 1 ± 0; p < 0.00001), and abnormal T2 weighted signal intensity (100% vs 11% patients; p=0.001) as compared to those without myocarditis. Interestingly, a significantly larger proportion of patients with myocarditis were males (95% vs 58%; p=0.02). Global native T1 values trended towards but did not reach statistical significance between the two groups (1058 ± 86 ms vs 1002 ± 72; p=0.09; figure 3). A cut-off of > 1200 ms for global native T1 measurement was found to be associated with the use of inotropes (100% vs 0%; p=0.006). In those with myocarditis, a negative correlation was seen between left ventricular ejection fraction (LVEF) and LGE, as well as LVEF and hs-TnT, but these did not reach statistical significance (R2=-0.05; p=0.8 and R2= -0.35; p=0.1, respectively).Discussion
Myocarditis has been documented to have a bimodal distribution in pediatric patients, with peaks in early childhood and in the teenage years4. Patients with moderate or severe LV dysfunction, younger age, and gastrointestinal symptoms at presentation may me at higher risk for prolonged LV dysfunction, cardiac transplant or death4-6. Biomarkers are needed for risk stratification in this vulnerable population.Prior studies in adults have shown higher levels of hs-TnT, LGE or lower LVEF to be predictors of poor outcome, including a composite endpoint of cardiac death, urgent heart transplant, and hospitalization for worsening heart failure2,6. Positive correlation between CMR, LVEF, and serum biomarkers of myocardial injury has been reported1,6,7. Both pediatric and adult studies have demonstrated CMR to be invaluable in increasing the sensitivity and accuracy of diagnosis, particularly when combined with hs-TnT5,8,9.
Our study was limited due to the heterogeneity of the diagnoses and small sample size but did show significant correlations between CMR biomarkers and hs-TnT, CMR biomarkers and myocarditis diagnosis, and between increased T1 signal and need for inotropic support.
Conclusion
There is a strong positive correlation between hs-TnT and LGE in pediatric patients with acute myocarditis, and these patients are significantly more likely to be male, show evidence of elevated T2 signal intensity, have a high hs-TnT, and have an increased LGE distribution than children undergoing CMR with elevated hs-TnT and other diagnoses. T1 cut-offs may be valuable in predicting need for inotropic support. Further studies are needed to assess predictive ability of these biomarkers on clinical outcomes.Acknowledgements
We would like to acknowledge our entire MRI technologist crew, including Steven Philip, Yuland Tyner, Shannon Scott, Neina Greenhouse, and Denia Torres.References
1. Kottwitz J, Bruno KA, Berg J, et al. Myoglobin for Detection of High-Risk Patients with Acute Myocarditis. J Cardiovasc Transl Res. 2020;13(5):853-863.
2. Sramko M, Kubanek M, Tintera J, et al. Utility of combination of cardiac magnetic resonance imaging and high-sensitivity cardiac troponin T assay in diagnosis of inflammatory cardiomyopathy. Am J Cardiol. 2013;111(2):258-264.
3. Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized Myocardial Segmentation and Nomenclature for Tomographic Imaging of the Heart: A Statement for Healthcare Professionals From the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539-542.
4. Butts RJ, Boyle GJ, Deshpande SR, et al. Characteristics of Clinically Diagnosed Pediatric Myocarditis in a Contemporary Multi-Center Cohort. Pediatr Cardiol. 2017;38(6):1175-1182.
5. Banka P, Robinson JD, Uppu SC, et al. Cardiovascular magnetic resonance techniques and findings in children with myocarditis: a multicenter retrospective study. J Cardiovasc Magn Reson. 2015;17:96.
6. Rodriguez-Gonzalez M, Sanchez-Codez MI, Lubian-Gutierrez M, Castellano-Martinez A. Clinical presentation and early predictors for poor outcomes in pediatric myocarditis: A retrospective study. World J Clin Cases. 2019;7(5):548-561.
7. Nadjiri J, Nieberler H, Hendrich E, et al. Performance of native and contrast-enhanced T1 mapping to detect myocardial damage in patients with suspected myocarditis: a head-to-head comparison of different cardiovascular magnetic resonance techniques. Int J Cardiovasc Imaging. 2017;33(4):539-547.
8. Kotanidis CP, Bazmpani MA, Haidich AB, Karvounis C, Antoniades C, Karamitsos TD. Diagnostic Accuracy of Cardiovascular Magnetic Resonance in Acute Myocarditis: A Systematic Review and Meta-Analysis. JACC Cardiovasc Imaging. 2018;11(11):1583-1590.
9. Patriki D, Gresser E, Manka R, Emmert MY, Luscher TF, Heidecker B. Approximation of the incidence of Myocarditis by Systematic Screening With Cardiac Magnetic Resonance Imaging. JACC Heart Fail. 2018;6(7):573-579.
Figures