1976
Histogram-based analysis of recurrence pattern correlations with MGMT methylation status in glioblastoma using synthetic MRI and 3D-ASL
Pei Dang1, Xueying Huang2, Xin Ge3, Lidong Wang4, Aijun Wang2, Minglei Wang2, Xuhong Yang5, Yuhui Xiong6, and Xiaodong Wang7
1Radiology, General Hospital of Ningxia Medical University, yinchuan, China, 2General Hospital of Ningxia Medical University, Yinchuan, China, 3Lanzhou University, Lanzhou, China, 4Radiology, Yinchuan Hospital of Traditional Chinese Medicine, Yinchuan, China, 5Ningxia Medical University, Yinchuan, China, 6GE Healthcare MR Research, Beijing, China, 7Radiology, General Hospital of Ningxia Medical University, Yinchuan, China
1Radiology, General Hospital of Ningxia Medical University, yinchuan, China, 2General Hospital of Ningxia Medical University, Yinchuan, China, 3Lanzhou University, Lanzhou, China, 4Radiology, Yinchuan Hospital of Traditional Chinese Medicine, Yinchuan, China, 5Ningxia Medical University, Yinchuan, China, 6GE Healthcare MR Research, Beijing, China, 7Radiology, General Hospital of Ningxia Medical University, Yinchuan, China
Synopsis
Keywords: Tumors, Cancer, Glioblastoma; Synthetic MRI; 3D-ASL; Histogram; MGMT; Recurrence patterns
At least 10% of glioblastoma relapses occur at distant and even contralateral locations. This disseminated growth limits surgical intervention and contributes to neurologicalmorbidity.The aim of the present study was to evaluate factors predicting the recurrencepattern determined.The results revealed that the pattern of recurrence in glioblastoma patients after combined radio-chemotherapy treated are strictly correlated with age at diagnosis and MGMT methylation status.Whole-tumor histogram analysis of quantitative parameters from synthetic MRI and 3D-ASL was to evaluate the value of predicting MGMT methylation status .Combining T110th, T210th ,and CBFentropy may explore as an effective strategy to predict of MGMT methylation status.Introduction
Glioblastoma (GBM) carries a poor prognosis primarily because of its high rate of recurrence1. Since GBM mostly recurs around the resection cavity, postoperative radiotherapy focuses on the margins of this cavity.Distant recurrence has been reported even when good control is achieved over the initial lesion2. This disseminated growth limits surgical intervention and contributes to neurological morbidity3.The ability to predict the recurrence pattern would be highly useful for determining effective treatment strategies. According to Alba A. Brandes,MGMT promoter methylation status was found to be correlated with the site of recurrence for GBM4. MGMT promoter methylation status obtained from biopsy tissue. However, biopsy only provide information of a small area of the tumor. Thus, noninvasive imaging makers for assessing heterogeneity in a tumor might be clinically beneficial. Synthetic MRI technique is a novel imaging method that provides simultaneous quantification of multiple relaxometry.Previous studies have reported Synthetic MRI application in the predict of IDH mutation in glioma5 and HER2 mutation in breast cancer6.3D-ASLuses magnetically labeled arterial blood as an endogenous tracer and offers non-invasive quantitative measurement of cerebral blood flow (CBF)7. Therefore, we herein investigated among the factors leading to the recurrence pattern and whether the combined histogram analysis of quantitative parameters from synthetic MRI and 3D-ASL is useful for predicting the MGMT methylation status.Materials and Methods
Patients:From August 2020 to July 2021, a total of 50 gliomas patients (28 men and 22 women; mean age, 45.02 ± 16.25 years) were confirmed by biopsy or surgical pathology enrolled in the study. The detailed for MGMT status assessment and definitions of recurrence patterns are shown in Fig.1.We defined “local recurrence”, a new enhanced lesion at or within 3 cm of the primary site resection cavity ,show in Fig. 2(1H).We defined “distant recurrence”, a new enhanced lesion centered more than 3 cm away from the primary site resection cavity or margin of the primary residual tumor8,show in Fig. 2(2H).Imaging parameters:All patients underwent MR exams with a 3.0T whole-body scanner (Signa Architect, GE, USA) with a 48-channel phased-array head coil.The scan sequences included synthetic MRI, ASL and contrast-enhanced T1FLAIR (T1FLAIR+C). Synthetic relaxometry T1map, T2map, PD maps and CBFmap were generated from the raw data produced by MAGIC sequence using a vendor-provided program (MAGiC, v. 100.1.1).The detailed acquisition parameters were as follows: (1)synthetic MRI: TR/TE = 4214/21.6ms, FOV = 240×240mm, matrix =160×166, slice thickness = 5 mm; acquisition time = 1 min and 11 s;(2)3D-ASL:TR/TE = 4854/53.5ms, FOV = 240×240mm, matrix =160×166, slice thickness = 4 mm; acquisition time = 3min and 22 s.
Data processing:These maps and T1FLAIR+C images were co-registered to T1 images using SPM12(www.fil.ion.ucl.ac.uk/spm).A 3D regions of interest (ROI) of the whole tumor (ROI ) was manually delineated on T1FLAIR+C images to include all hyperintense regions.Using ITK-SNAP(http://www.itksnap.org/pmwiki/pmwiki.php),show in Fig.2(1F,2F).Finally, all voxels within ROI were extracted from maps to obtain the histogram-based features, including mean, kurtosis,skewness, entropy,10th and 90th percentiles.
Statistical analysis:Statistical analysis of the data was performed using MedCalc for Windows (v. 26.0, Chicago, IL, USA / v. 20.009, Ostend, Belgium). The Student’s t-test, Mann-Whitney U-test or Fisher’s exact test was used to compare the parameters between groups. Receiver operating characteristic (ROC) curves (AUC) were also evaluated to assess the diagnostic value of parameters for prediction.A p-value< 0.05 was considered significant.
Results
- The pattern of recurrence in glioblastoma are correlated with age and MGMT methylation status respectively (p<0.05,p<0.05), detailed results shown in Table 1.
- The T110th,T210th and CBFentropy in MGMT methylated (+) group is significantly lower than that MGMT unmethylated (-) group respectively(p<0.01,p=0.005,p<0.01),detailed results shown in Table 2.
- The differentiation ability of predicting the MGMT methylation status with T110th, T210th,and CBFentropy are summarized in the ROC curves shown in Fig.3.Combination of three parameters (T110th+T210th+CBFentropy) have the highest AUC (0.973), as well as the sensitivity and specificity among all combined parameters.
Discussion
In the present study, distant recurrence was observed in 13% (6/45)of patients, and MGMT methylation status correlated with the pattern of recurrence, which confirmed the findings of the previous studies9. It is unclear whether the combined chemoradiation approach, by having a synergistic effect on MGMT methylated cells, can enhance local GBM cell eradication. The latter hypothesis is supported by our finding that MGMT methylation was associated with distant recurrence rates(28%,5/13). This suggests that preoperative non-invasive prediction of MGMT is very important for the evaluation pattern of recurrence. In this study, we investigated histogram-based analysis of quantitative MR parameters including T1, T2, PD, and CBF in predicting the MGMT methylation status. The results revealed that lower T110th, T210thand CBFentropy in MGMT methylation than in MGMT unmethylation, furthermore, quantitative multi-parameters of T110th+ T210th+ CBFentropy improved the prediction performance. To reduce biases caused by subjective factors during ROIs selection, we delineated a 3D whole-tumor ROI on T1FLAIR+C images from which histogram-based T1map, T2map, PD maps, and CBFmap features were extracted. Of note, as none of synthetic MRI and 3D-ASL rely on exogenous contrast or tracers, would be beneficial for those with gadolinium contrast agent allergy or decreased renal function.Conclusion
Histogram-based analysis by using synthetic MRI and 3D-ASL may be useful and noninvasive clinical markers for predicting the MGMT methylation, status, thereby predicting recurrence patterns and improving prognosis.Acknowledgements
Thanks to the Department of Radiology, General Hospital of Ningxia Medical University for the equipment provided and Professor Wang Xiaodong for the guidance.References
- DeWitt JC, Mock A, Louis DN. The 2016 WHO classification of central nervous system tumors: what neurologists need to know. Curr Opin Neurol. 2017;30(6):643-649.
- Parsa AT, Wachhorst S, Lamborn KR, et al. Prognostic significance of intracranial dissemination of glioblastoma multiforme in adults. J Neurosurg. 2005;102(4):622-628.
- Wick W, Stupp R, Beule AC, et al. A novel tool to analyze MRI recurrence patterns in glioblastoma. Neuro Oncol. 2008;10(6):1019-1024.
- Brandes AA, Franceschi E, Paccapelo A, et al. Role of MGMT Methylation Status at Time of Diagnosis and Recurrence for Patients with Glioblastoma: Clinical Implications. Oncologist. 2017;22(4):432-437.
- Kikuchi K, Togao O, Yamashita K, et al. Quantitative relaxometry using synthetic MRI could be better than T2-FLAIR mismatch sign for differentiation of IDH-mutant gliomas: a pilot study. Sci Rep. 2022;12(1):9197. Published 2022 Jun 2.
- Li Q, Xiao Q, Yang M, et al. Histogram analysis of quantitative parameters from synthetic MRI: Correlations with prognostic factors and molecular subtypes in invasive ductal breast cancer. Eur J Radiol. 2021;139:109697.
- Alsaedi A, Doniselli F, Jäger HR, et al. The value of arterial spin labelling in adults glioma grading: systematic review and meta-analysis. Oncotarget. 2019;10(16):1589-1601. Published 2019 Feb 22..
- Shibahara I, Sonoda Y, Saito R, et al. The expression status of CD133 is associated with the pattern and timing of primary glioblastoma recurrence. Neuro Oncol. 2013;15(9):1151-1159.
- Niyazi M, Schnell O, Suchorska B, et al. FET-PET assessed recurrence pattern after radio-chemotherapy in newly diagnosed patients with glioblastoma is influenced by MGMT methylation status. Radiother Oncol. 2012;104(1):78-82.
Figures
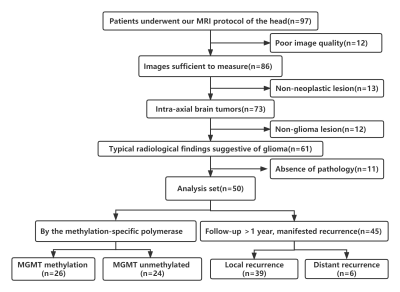
Fig.1 The flowchart of patient enrollment.
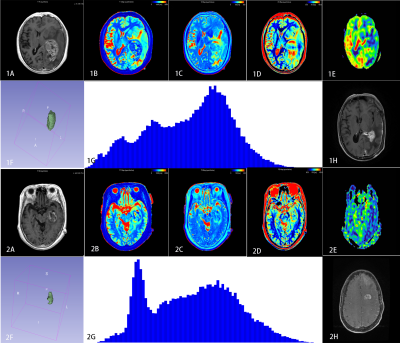
Fig.2 1A-1H:47-year-old glioblastoma with MGMT unmethylationtrue.Primary enhancement of lesions (1A), The quantitative parametric maps (T1, T2, PD and CBF) from synthetic MRI and 3D-ASL(1B-1E);3D-ROI(1F);histogram(1G);Three months later,local recurrence(1H).2A-2H:53-year-old glioblastoma with MGMT methylationtrue.Primary enhancement of lesions (2A), The quantitative parametric maps (T1, T2, PD and CBF) from synthetic MRI and 3D-ASL(2B-2E);3D-ROI(2F);histogram(2G);Six months later,distant recurrence(2H).
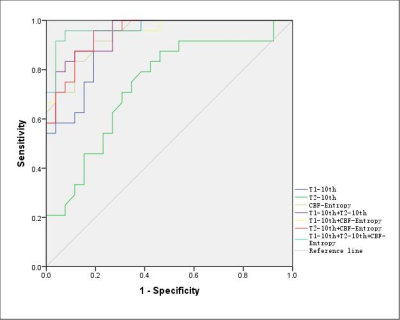
Fig.3 The ROC of T110th, T210th, CBFentropy ,T110th+ T210th,T110th+CBFentropy,T210th+CBFentropy and T110th+ T210th+ CBFentropyvalues for predicting the MGMT methylation. The AUC of T110th+ T210th+ CBFentropy (0.973) is significantly higher than T110th+ T210th (0.932), T110th+CBFentropy(0.919), and T210th+CBFentropy (0.890) (P = 0.0013, 0.0011, respectively).
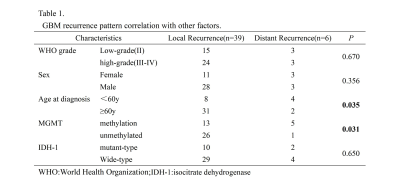
Table 1.GBM recurrence pattern correlation with other factors.
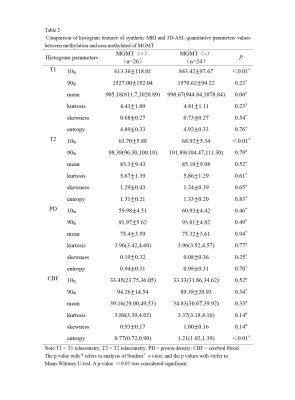
Table 2.Comparison of histogram features of synthetic MRI and 3D-ASL quantitative parameters values between methylation and non-methylated of MGMT.
DOI: https://doi.org/10.58530/2023/1976