1974
Correlation of MRI Radiomics Features and Recurrence After Gamma Knife Treatment in Parasagittal and Falx Meningiomas1Institute of Biomedical Engineering, Boğaziçi University, İstanbul, Turkey, 2Department of Radiation Oncology, Acıbadem University, İstanbul, Turkey, 3Department of Neurosurgery, Acıbadem University, İstanbul, Turkey, 4Brain Tumor Research Group, Acıbadem University, İstanbul, Turkey, 5Department of Radiology, Acıbadem University, İstanbul, Turkey
Synopsis
Keywords: Tumors, Radiomics, Gamma Knife, meningioma
Meningiomas located at and around the falx and superior sagittal sinus are known to have a more aggressive clinical behavior. Additionally, their localization and invasion characteristics make complete resection difficult, creating a need for radiosurgery. This study assessed the relationship between radiomics/clinical features of parasagittal and falx meningiomas and their recurrence-free survival after Gamma Knife. The radiomics and clinical features (age, pre-op tumor volume, coverage, and sensitivity) were analyzed together. Univariable Cox analysis associated maximum and skewness of T1 lesion, age, TV, and coverage, whereas multivariable Cox analysis associated skewness of T2 lesion, coverage, and selectivity with RFS.Introduction
Meningiomas are the most frequent primary intracranial neoplasm, and around 25% of all meningiomas are located along the parasagittal and falx regions.1 Parasagittal and falx meningiomas (PFM) are located around vital venous structures, which precludes a complete surgical resection. Therefore, residual tumors after surgery, regrowth, or recurrences are more common in PFM than in other anatomical localizations.2 Gamma Knife (GK) radiosurgery is a valid and effective treatment modality in these situations.3 Herein, we investigated the relationship of radiomics and clinical features (age, pre-op tumor volume, coverage, sensitivity) with the recurrence-free survival (RFS) of PFM after GK radiosurgery.Methods
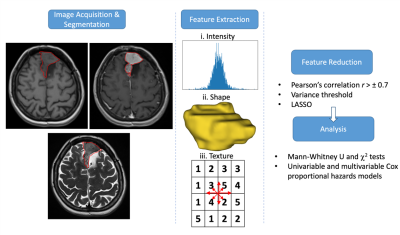
We retrospectively collected data from 105 PFM (m/f: 0.48, age: 54±12 years, nine local recurrences). Pre-GK brain protocol, including pre- and post-contrast T1-weighted MRI (T1w, TR/TE= 2080/2.67ms) and T2-weighted MRI (T2w, TR/TE= 7640/107ms), were acquired using a 3T clinical MRI scanner (Siemens Healthcare, Erlangen, Germany). The radiomics workflow of the study is given in Fig. 1. First, the contrast-enhancing (T1) and T2 hyperintense (T2) tumor volumes were manually segmented by the neurosurgeon. Then, a 100-gray-level normalization scale was applied to MR images. To minimize the effect of inhomogeneity between acquisitions, images were z-score normalized and resampled to the same resolution (1×1×1 mm3). From each modality, 1132 radiomics features were extracted, including first-order statistics, shape, and texture using PyRadiomics.4 A pairwise Spearman’s correlation filter (r>±0.7), low variance threshold, and least absolute shrinkage operator (LASSO) were consecutively applied to identify the features most predictive of RFS. The differences between recurrent and non-recurrent meningiomas in terms of selected radiomics, age, pre-op tumor volume (TV), coverage, and selectivity were assessed by Mann-Whitney U tests, while Chi-square tests were used to assess the differences of sex and the multiplicity of tumors. Univariable and multivariable Cox proportional hazards models were applied to identify the significant factors related to recurrence.Results
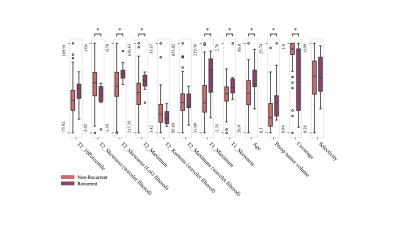
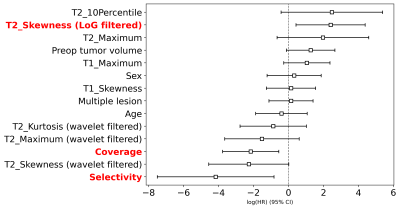
Sex distributions and multiplicity of tumors didn’t significantly differ between the recurrent and non-recurrent PFM patients (P=0.6 and P=0.54, respectively). Recurrent patients presented at a significantly higher age and higher pre-op TV and lower coverage compared to non-recurrent patients (P<0.05, Fig.2). Five radiomics features significantly differed in recurrent and non-recurrent groups (P<0.05, Fig.2). While recurrent patients presented significantly higher T2 skewness (Laplacian of Gaussian (LoG) filtered), T2 maximum, T1 maximum, and T1 skewness, they had lower T2 skewness (wavelet filtered) compared to non-recurrent patients. Table 1 shows the results of univariable and multivariable Cox analyses for RFS of PFM. Univariable Cox analysis associated higher maximum and skewness of T1 lesion volume, age, pre-op TV, and lower coverage (P<0.05 for all) with shorter RFS. On the other hand, lower skewness of T2 lesion volume (with LoG filtering), and higher coverage and selectivity were significantly associated with a longer RFS in multivariable Cox analysis (P<0.05 for all, Fig.3).Discussion
According to the results, the combination of radiomics features extracted from the pre-GK anatomical MRI and the clinical parameters were associated with recurrence in PFM after GK radiosurgery. In literature, standard MRI findings, such as an irregular shape,5 high peritumoral edema,6 and the extent of tumor resection,7 have been associated with recurrence; however, quantitative assessments of MR images may add valuable information about the patient prognosis. Thus, radiomics offer objective and quantitative features to build prognostic models. A previous multimodal study showed that the radiomics features, such as T1 max probability, T1 cluster shade, and ADC correlation, could predict recurrence in skull base meningiomas.8 In our study, higher T1 maximum, T1 skewness, age, pre-op tumor volume, and lower coverage were associated with shorter PFS. A higher T1 maximum may be a clue of bleeding, which appears as hyperintense in T1w MRI, whereas higher T1 skewness could indicate intensity asymmetry from a normal distribution. On the other hand, lower T2 skewness and higher coverage and selectivity were associated with longer PFS.Conclusion
The combination of radiomics and clinical features might help to identify PFM patients with a high risk of recurrence after GK and could improve clinical decision-making.Acknowledgements
No acknowledgement found.References
1. American Society of Clinical Oncology (ASCO). Meningioma. Published online 2022. Accessed May 13, 2022. https://www.cancer.net/cancer-types/meningioma/view-all#:$\sim$:text=Falx and parasagittal meningioma.,the inside of the skull.
2. Pinzi V, Fariselli L, Marchetti M, Scorsetti M, Navarria P. Stereotactic radiotherapy for parasagittal and parafalcine meningiomas: Patient selection and special considerations. Cancer Manag Res. 2019;11:10051-10060. doi:10.2147/CMAR.S187371
3. Hasegawa T, Kida Y, Yoshimoto M, Iizuka H, Ishii D, Yoshida K. Gamma knife surgery for convexity, parasagittal, and falcine meningiomas: Clinical article. J Neurosurg. 2011;114(5):1392-1398. doi:10.3171/2010.11.JNS10112
4. van Griethuysen JJMM, Fedorov A, Parmar C, et al. Computational radiomics system to decode the radiographic phenotype. Cancer Res. 2017;77(21):e104-e107. doi:10.1158/0008-5472.CAN-17-0339
5. Ildan F, Erman T, Göçer AI, et al. Predicting the probability of meningioma recurrence in the preoperative and early postoperative period: A multivariate analysis in the midterm follow-up. Skull Base. 2007;17(3):157-171. doi:10.1055/s-2007-970554
6. Hwang WL, Marciscano AE, Niemierko A, et al. Imaging and extent of surgical resection predict risk of meningioma recurrence better than WHO histopathological grade. Neuro-Oncol. 2016;18(6):863-872. doi:10.1093/neuonc/nov285
7. Nanda A, Bir SC, Konar S, et al. Outcome of resection of WHO Grade II meningioma and correlation of pathological and radiological predictive factors for recurrence. J Clin Neurosci. 2016;31:112-121. doi:10.1016/j.jocn.2016.02.021
8. Zhang Y, Chen JH, Chen TY, et al. Radiomics approach for prediction of recurrence in skull base meningiomas. Neuroradiology. 2019;61(12):1355-1364. doi:10.1007/s00234-019-02259-0
Figures