1973
The efficacy of preoperative MRI features in the diagnosis of meningioma WHO grade and brain invasion1Shenzhen Second People's Hospital, Shenzhen, China, 2Philips Healthcare, Guangzhou, China, 3The First Affiliated Hospital of Jinan University, Guangzhou, China
Synopsis
Keywords: Tumors, MR Value
The purpose of this study is to explore the efficacy of clinical and MRI-specific features for tumor grading and the brain invasion assessment in patient with meningioma. Our results showed that the tumor-brain interface is considered as a key factor, preoperative MRI has excellent performance in diagnosing meningioma WHO grade and brain invasion.Introduction
Meningioma is one of the most common brain tumors, accounting for 37.6% of primary intracranial tumors[1].WHO grade 1 meningiomas have a very low recurrence rate after total resection. However, with the increase of WHO grade of meningioma, the recurrence tendency increased[2]. Besides, meningiomas with brain invasion exhibit aggressive behaviors, an increased recurrence rate, and an increased risk of postoperative seizures as well as postoperative bleeding[3-4]. Therefore, it is important to propose a non-invasion, efficient, and reliable approach for the evaluation of tumor grade and brain invasion in meningioma. To our knowledge, the imaging biomarkers of brain invasion are still unclear. Here, we aimed to explore the efficacy of clinical and MRI-specific features for tumor grading and the brain invasion assessment in patient with meningioma.Materials and methods
675 patients with meningioma(108 with brain invasion) who underwent meningiomas resected in our hospital from 2006 to 2022, were retrospectively enrolled in this study. MRI data including T1WI, T2WI, DWI and contrast-enhanced T1WI (CE-T1WI) were acquired on a 3.0T MRI scanner (Ingenia; Philips Medical Systems, Best, The Netherlands). Two senior neuroradiologists who blinded to the pathological findings analyzed the conventional MRI characteristics according to the 2022 edition of the WHO guidelines. For the ADC analysis, the slice with the maximum tumor was selected and five ROIs were placed on the sloid portion of the tumor. The average ADC value of five ROIs was calculated and a total of 17 features were acquired. Pathological findings, which is the gold standard for the tumor grading and brain invasion assessment in meningioma, were reinterpreted by two neuropathologists referring to the 2022 CNS WHO guideline. The univariate logistic regression was performed to determine the independent risk factors for meningioma WHO grading and brain invasion assessment. And then the significant factors were further selected for multivariate logistic regression analysis. The diagnostic efficacy was analyzed using the receiver operator characteristic curve (ROC), and the area under the curve (AUC), sensitivity and specificity were calculated. The statistical analysis was performed with SPSS version 26.0 software, and a p value < 0.05 was considered statistically significant.Results
Univariate logistic regression analysis showed that sex, tumor size, lobulated sign, peritumoral edema, vascular flow void, bone invasion, tumor-brain interface, finger-like protrusion and mushroom sign were significant factors for meningioma WHO grading, while sex, tumor size, lobulated sign, peritumoral edema, ADC value, vascular flow void, bone invasion, tumor-brain interface, finger-like protrusion and mushroom sign were significant factors for predicting brain invasion. Multivariable logistic regression analysis showed that the lobulated sign, tumor-brain interface, finger-like protrusion, mushroom sign and bone invasion were independent risk factors for diagnosing meningioma WHO Grades(Figure 1), while tumor size, ADC value, lobulated sign, tumor-brain interface, finger-like protrusion, mushroom sign and bone invasion were independent risk factors for diagnosing brain invasion (P < 0.05) (Figure 2-3). The tumor-brain interface had the highest efficacy in evaluating WHO grade and brain invasion, with AUCs of 0.779 and 0.860, respectively(Figure 4). The fitting variables obtained by multivariate logistic regression had AUCs of 0.834 and 0.935 for determining WHO grade and brain invasion, respectively.Conclusions
Preoperative MRI has excellent performance in diagnosing meningioma WHO grade and brain invasion, while the tumor-brain interface is considered as a key factor. The preoperative MRI characteristics of meningioma can help predict WHO grade and brain invasion, which may improve the resection efficacy for the tumor and invaded brain tissue, reduce recurrence and mortality rates, as well as improve patient prognosis to some extent.Acknowledgements
No acknowledgement found.References
1. Euskirchen P, Peyre M. Management of meningioma. Presse Med 2018; 47:e245-e252.
2. Huntoon K, Toland A, Dahiya S. Meningioma: A Review of Clinicopathological and Molecular Aspects. Front Oncol 2020; 10:579599.
3. Bulleid LS, James Z, Lammie A, Hayhurst C, Leach PA. The effect of the revised WHO classification on the incidence of grade II meningioma. Br J Neurosurg 2020; 34:584-586.
4. Hess K, Spille DC, Adeli A, et al. Brain invasion and the risk of seizures in patients with meningioma. J Neurosurg 2018; 130:789-796.
Figures
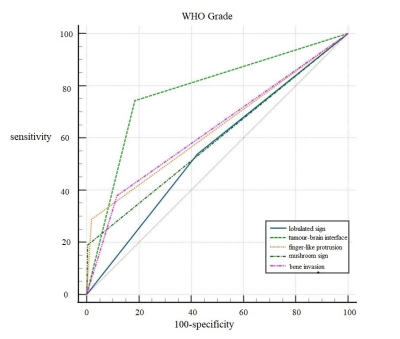
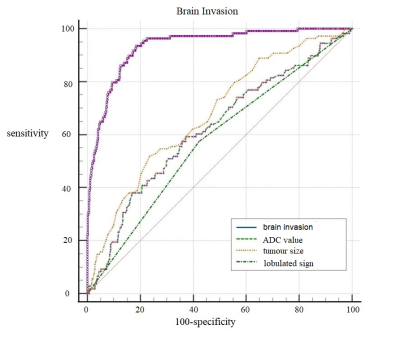
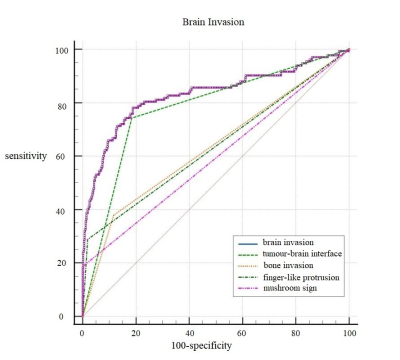
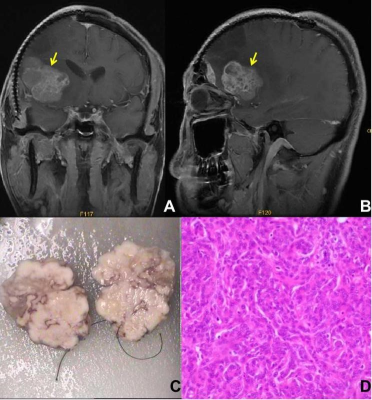
Figure 4: Illustrative example of the "tumor-brain interface" variable.
A, B. Enhanced T1WI sequence, arrow shows an unclear tumor-brain interface.
C. Adhesion of peripheral brain tissue was recorded during surgery, and the brain tissue around the tumor was sampled.
D. Pathological examination confirmed brain invasion.