1957
Association between diffusion-weighted image analysis along the perivascular space index and early-onset post‑stroke cognitive impairment
Hongwei Li1, Min Chu2, Lianlian Liu3, He Wang1,4,5, and Jing Zhao2
1Institute of Science and Technology for Brain-Inspired Intelligence, Fudan University, Shanghai, China, 2Department of Neurology, Minhang Hospital, Fudan University, Shanghai, China, 3Department of Radiology, Minhang Hospital, Fudan University, Shanghai, China, 4Human Phenome Institute, Fudan University, Shanghai, China, 5Key Laboratory of Computational Neuroscience and Brain-Inspired Intelligence (Fudan University), Ministry of Education, Shanghai, China
1Institute of Science and Technology for Brain-Inspired Intelligence, Fudan University, Shanghai, China, 2Department of Neurology, Minhang Hospital, Fudan University, Shanghai, China, 3Department of Radiology, Minhang Hospital, Fudan University, Shanghai, China, 4Human Phenome Institute, Fudan University, Shanghai, China, 5Key Laboratory of Computational Neuroscience and Brain-Inspired Intelligence (Fudan University), Ministry of Education, Shanghai, China
Synopsis
Keywords: Stroke, Neuroscience
The mechanism of cognitive impairment following stroke is uncertain. It has been demonstrated that the glymphatic system has an impact on cognitive function, which can be measured by the diffusion weighted image analysis along the perivascular space (DWI-ALPS) index. The purpose of this study was to see whether the DWI-ALPS index was associated with early-onset post-stroke cognitive impairment. Our data revealed that DWI-ALPS index in PSCI group was significantly lower than in non-PSCI group, and it had a good predictive value for PSCI.Introduction
Stroke is a frequent condition characterized by high morbidity, disability, and mortality1. Post-stroke cognitive impairment (PSCI) is a frequent consequence and one of the main factors lowering quality of life2. It has been shown that cognitive impairment (CI) within 7 days following stroke could predict mortality, long-term cognitive outcomes, and functional outcomes3. Finding more precise markers to help identify patients who are more prone to experience early PSCI is urgently needed. The glymphatic system, which contributes to amyloid-beta protein (Aβ) deposition and the development of CI, was recently discovered4. Nonetheless, it has difficulty directly evaluating the function of the glymphatic system in the human body. Taoka et al. proposed a new index based on diffusion weighted image analysis along the perivascular space (DWI-ALPS)5. DWI sequence requires short imaging time and is widely used in clinical practice. Accordingly, we aimed to explore whether DWI-ALPS index was associated with early-onset PSCI.Materials and methods
Data acquisitionWe prospectively enrolled 29 consecutive patients with acute ischemic stroke (AIS) who were admitted to the Neurology Department of Minhang Hospital. Patients were excluded if they had central nervous system diseases history, cancer, liver dysfunction, renal insufficiency, cognitive impairment or dementia before stroke. All patients were divided into the PSCI group and non-PSCI group according to the Mini-Mental State Examination (MMSE) within 2 weeks after stroke. MRI studies were performed on a 3 T scanner (uMR 770, Shanghai United Imaging Healthcare, Shanghai, China) equipped with an 24-channel head& neck coil. The parameters of DWI clinical sequence were as follows: TR=4287ms; TE=98.6ms, FOV=230×200mm, slice thickness=5.0mm, motion-probing gradient= 3 axes, number of averages=1 for b=0 and 2 for b=1000. The slices were positioned parallel to the anterior commissure-posterior commissure line.
Image processing
Apparent diffusion coefficient (ADC) images in the x-axis, y-axis and z-axis were calculated from the DWI b0 and b=1000 images of the x-, y- and z-axis. The mean ADC were defined by averaging ADCs in all three directions and were used to predict the infarct volume (ADC<620×10-6mm2/s). The SWI images were aligned to DWI space and fused with the ADC images in order to see medullary veins clearly. As shown in Figure 2, the four ROIs were manually defined on the fusion images. The DWI-ALPS index was calculated according to the equation in Figure 2. SPSS (version 26.0, IBM Corp, Armonk, NY, USA) was applied for the association between DWI-ALPS and PSCI. Statistical significance was defined as P < 0.05 (two‐sided).
Results
As shown in Figure 1, among 29 patients, 15 developed PSCI. The DWI-ALPS index of the PSCI group was significantly lower than that of the non-PSCI group (P=0.002) (Figure 3). After adjusting for four risk factors (age, education, NHISS score and infarct volume) this difference remained significant (95%CI<0.001-0.484, P=0.020) (Table 1). Receiver operating characteristic (ROC) curve demonstrated that DWI-ALPS had a high predictive value of PSCI [area under the curve (AUC)=0.848, 95%CI=0.666-0.953, P<0.001] (Figure 4). Our finding indicated that glymphatic system dysfunction is independently associated with PSCI.Discussion and Conclusion
Our study found that the decline in the DWI-ALPS index was independently related to PSCI, suggesting that glymphatic system dysfunction might be involved in the development of PSCI. This may be due to the brain glymphatic system, which performs the task of removing brain waste and is crucial for maintaining normal cognitive function. To the best of our knowledge, no research has examined whether the DWI-ALPS index, which represents glymphatic system function, could be a valuable marker to assess early-onset PSCI. Therefore, our findings contribute to a better understanding of glymphatic system in PSCI.Acknowledgements
This study was supported by the National Natural Science Foundation of China (No. 82173646 and No.81973157), Natural Science Foundation of Shanghai (No.17dz23 08400) .References
1. Collaborators, G.S. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. Neurology 20, 795-820 (2021).2. Brainin, M., et al. Post-stroke cognitive decline: an update and perspectives for clinical research. Eur J Neurol 22, 229-238, e213-226 (2015).
3. Zietemann, V., et al. Early MoCA predicts long-term cognitive and functional outcome and mortality after stroke. Neurology 91, e1838-e1850 (2018).
4. Reeves, B., et al. Glymphatic System Impairment in Alzheimer's Disease and Idiopathic Normal Pressure Hydrocephalus. Trends in molecular medicine 26, 285-295 (2020).
5. Taoka, T., et al. Diffusion-weighted image analysis along the perivascular space (DWI-ALPS) for evaluating interstitial fluid status: age dependence in normal subjects. Jpn J Radiol 40, 894-902 (2022).
Figures
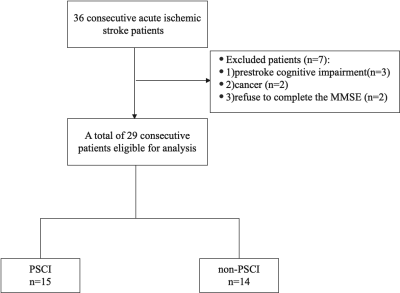
Figure
1.
Diagram of the study recruitment.
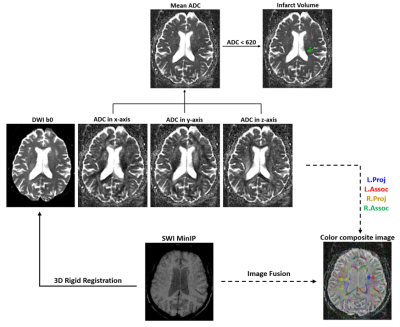
Figure
2. Flowchart
of DWI-ALPS index calculation. The Mean ADC was obtained by averaging the ADC
images in the x, y, z directions. The SWI images were aligned to DWI space and
fused with the ADC images in all three directions. The projection and association
fiber ROIs were manually identified on the fusion images. DWI-ALPS index=mean
(ADCxproj, ADCxassoc)/mean (ADCyproj, ADCzassoc).
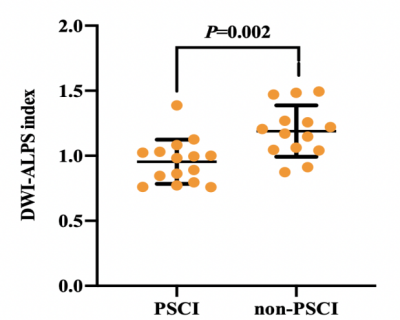
Figure
3.
DWI-ALPS index in PSCI and non-PSCI patients
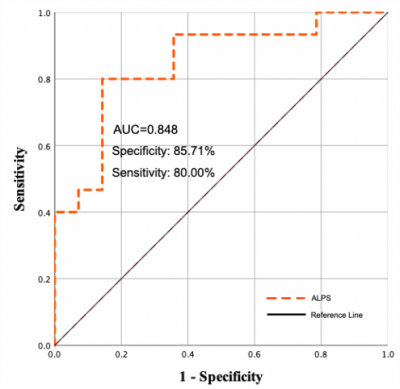
Figure 4. ROC
curve demonstrating the predictive ability of DWI-ALPS for PSCI
(The diagnostic efficacy of DWI-ALPS index for PSCI was
analyzed with a ROC analysis. The best threshold was 1.03, which resulted in a
sensitivity of 80.0% and a specificity of 85.71%, with an AUC of 0.848 (95% CI,
0.666–0.953, P< 0.001)
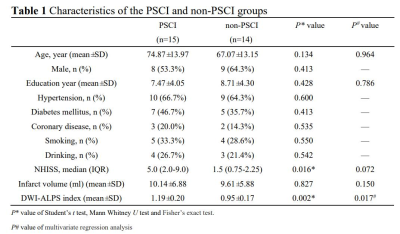
Table
1. Characteristics
of the PSCI and non-PSCI groups
DOI: https://doi.org/10.58530/2023/1957