1947
Prognostic value of the baseline magnetic resonance score with acute posterior circulation ischemic stroke after mechanical thrombectomy
huang shan shan1
1Xi’an No.1 Hospital, Xi'an, China
1Xi’an No.1 Hospital, Xi'an, China
Synopsis
Keywords: Stroke, Thrombo-Embolic
To investigate the predictive value of baseline DWI-pcASPECTS combined with MRA-collateral circulation score in patients with acute posterior circulation ischemic stroke after mechanical thrombectomy. DWI-pcASPECTS score and MRA-collateral circulation score before treatment were retrospectively analyzed in patients with acute posterior circulation ischemic stroke after mechanical thrombolectomy. Multivariate Logistic regression was used to analyze the independent predictors of functional outcomes 90 days after mechanical thrombectomy. MR-pcASCO score can be used as an important means to predict the prognostic function of patients with acute posterior circulation ischemic stroke after mechanical thrombectomy.Purpose
To investigate the prognostic value of the composite MR-pcASCO score, which combines the DWI-pcASPECTS and the MRA-collateral circulation score, at baseline among patients with acute posterior circulation ischemic stroke after mechanical thrombectomy.Methods
We retrospectively analyzed patients with acute posterior circulation ischemic stroke in a comprehensive stroke center in northern China from July 2021 to March 2022 and continuously collected patient information that met the inclusion criteria. The included patients met the diagnostic criteria of acute ischemic stroke in the Chinese guidelines for the diagnosis and treatment of acute ischemic stroke 2020. The inclusion criteria were as follows: (1) age ≥ 18 years old; (2) acute posterior circulation ischemic stroke, DWI and MRA were assessed at baseline; (3) occlusion or severe stenosis of the vertebral basilar artery or its branches; and (4) patients who underwent DSA and mechanical thrombectomy. The exclusion criteria were as follows: (1) intracranial hemorrhage or other intracranial lesions; (2) incomplete imaging data; (3) acute ischemic stroke in the anterior circulation; and (4) scores affected by other factors. All patients underwent an MRI examination after admission and before thrombectomy treatment. The MRI data were acquired on a 1.5T MR scanner (MAGNETOM Avanto, Siemens Healthineers, Erlangen, Germany) with a 32-channel receiver array head coil. A readout-segmented echo-planar DWI sequence were performed with following parameters: TR/TE=3250/77(126) ms, b value =0 ,1000 s/mm2, matrix=192*192, FOV =230*230 mm2, slice thickness=5mm, and slice gap=1.5 mm. The scanning parameters about the 3D-TOF-MRA sequence were as follows: TR/TE=22/7ms, matrix=320*320, FOV=240*240 mm2, and voxel size=0.6mm isotropic scanning. The scan range included the intracranial segment of the posterior circulation.In this study, the DWI-pcASPECTS was combined with the MRA-collateral circulation score to define the composite score, i.e., the MR-pcASCO score, which has a maximum score of 20, including 10 points on the pcASPECTS and 10 points on the collateral circulation score. The scores were determined by two experienced neuroimaging doctors.Statistical analysis was performed using SPSS version 26 (IBM, Armonk, New York, USA). Continuous data are described as the mean ± SD and were compared using independent-samples T-tests or Mann-Whitney U-tests, while categorical variables are presented as a frequencies(percentages) and were compared using the chi-squared test. To minimize overfitting of the regression model, multicollinearity of pretreatment variables (baseline and imaging parameters) in univariate analysis with p<0.05 was assessed using the variance inflation factor (VIF). Variables with a VIF <10 were included in the multivariate binary logistic regression. A nomogram was constructed from the results of the multivariate analysis using the R package Version 3.4.4 (R Package for Statistical Computing; www.r-project.org). Receiver operating characteristic (ROC) analysis and the area under the curve (AUC) were used to assess and compare prognostic models. The Youden index was computed using sensitivity + specificity − 1 to identify the optimal cutoff values. The Delong test was used to compare the diagnostic performance of the ROC curve. A two-tailed p<0.05 was considered statistically significant.Results
Mechanical thrombectomy was performed in 57 patients; 38 patients had a good prognosis, 19 patients had a poor prognosis, 6 patients died, and 33 patients were successfully recanalized. Multivariate logistic regression showed that the GCS score (OR:2.14, 95% CI: 1.15-3.95, P =0.016) and pcASCO score (OR:0.74, 95% CI: 0.25-2.18, P =0.04) were independent predictors of good functional outcome. Based on ROC curve analysis, the discriminant ability of functional independence classification with the pcASCO score≥14.5 (AUC 0.81, 95% CI: 0.67-0.94) was higher than that of the pcASPECTS (AUC 0.65) and collateral circulation score (AUC 0.79). ROC curve analysis also showed that the diagnostic efficacy of the pcASCO score (AUC 0.80, 95% CI: 0.63-0.97) was slightly higher than that of the GCS score (AUC 0.76, 95% CI: 0.56-0.95) in the group with a low baseline GCS score.Discussion
We combined DWI-pcASPECTS in brain tissue regional and MRA-collateral circulation scores to comprehensively evaluate the baseline infarction of patients. We have reliable data to confirm that the baseline GCS score and MR-pcASCO score are independent predictors of good functional outcome and have good diagnostic efficacy. ROC curve analysis revealed that the optimal cutoff point of the baseline GCS score is 13.5, and the higher the score is, the better the prognosis of patients. This finding suggests that the baseline status of patients is closely related to the prognosis. DWI-pcASPECTS or MRA-collateral circulation score alone. This research result may improve the prediction of prognosis. It can be used as a simple auxiliary means for the classification of patients with vertebrobasilar artery occlusion, especially when the indication for mechanical thrombectomy is uncertain. In patients with poor baseline GCS scores (GCS<13.5), the MR-pcASCO score was slightly more effective than the GCS score. The MR-pcASCO score may be a practical and easy-to-implement method to predict outcomes.Conclusion
The composite MR-pcASCO score can be used as an important predictor of the prognosis of patients with acute posterior circulation ischemic stroke after mechanical thrombectomy.Acknowledgements
All authors made substantial contributions to this manuscript and take responsibility for its content. YL and JY was responsible for the study design. YY, YG, TL, XS, XX, GL, HS, HH contributed to the acquisition of MRI and demographical data. SH and BB performed the data analysis. SW and ZL assisted with data analysis and interpretation of findings. SH drafted the manuscript. BB provided critical revision of the manuscript for important intellectual content. All authors critically reviewed content and approved final version for publication.References
1.AusmanJ ,Liebeskind D , Gonzalez N , et al. A review of the diagnosis and management of vertebral basilar (posterior) circulation disease[J]. Surgical Neurology International, 2018, 9(1):106.2.OheY ,Dembo T , Horiuchi Y , et al. Clinical review of 28 patients with basilar artery occlusion.[J]. Journal of Stroke & Cerebrovascular Diseases, 2013, 22(4):358-363.
3.Liu X , Xu G , Liu Y , et al. Acute basilar artery occlusion: Endovascular Interventions versus Standard Medical Treatment (BEST) Trial-Design and protocol for a randomized, controlled, multicenter study.[J]. International Journal of Stroke Official Journal of the International Stroke Society, 2017:1747493017701153.
4.Endovascular Therapy for Stroke Due to Basilar-Artery Occlusion[J]. The Journal of Emergency Medicine, 2021(20).
5.ZiW ,Qiu Z , Wu D , et al. Assessment of Endovascular Treatment for Acute Basilar Artery Occlusion via a Nationwide Prospective Registry[J]. JAMA Neurology, 2020, 77(5).
6.Kniep H C ,Sporns P B , Broocks G , et al. Posterior circulation stroke: machine learning-based detection of early ischemic changes in acute non-contrast CT scans[J]. Journal of Neurology, 2020, 267(4).
7.Fahed R , Lecler A , Sabben C , et al. DWI-ASPECTS (Diffusion-Weighted Imaging–Alberta Stroke Program Early Computed Tomography Scores) and DWI-FLAIR (Diffusion-Weighted Imaging–Fluid Attenuated Inversion Recovery) Mismatch in Thrombectomy Candidates[J]. Stroke, 2017:STROKEAHA.117.019508.
8.Piedade G S ,Schirmer C M , Goren O , et al. Cerebral Collateral Circulation: A Review in the Context of Ischemic Stroke and Mechanical Thrombectomy[J]. World Neurosurgery, 2018, 122:33-42.
9.BroocksGabriel,MeyerLukas,Faizy Tobias D et al. New imaging score for outcome prediction in basilar artery occlusion stroke.[J] .EurRadiol, 2022, 32: 4491-4499.
10.Puetz V , Sylaja P N , Coutts S B , et al. Extent of Hypoattenuation on CT Angiography Source Images Predicts Functional Outcome in Patients With Basilar Artery Occlusion[J]. Stroke, 2008.
11.Takeshi, Yoshimoto, Manabu, et al. Use of Diffusion-Weighted Imaging-Alberta Stroke Program Early Computed Tomography Score (DWI-ASPECTS) and Ischemic Core Volume to Determine the Malignant Profile in Acute Stroke.[J]. Journal of the American Heart Association, 2019, 8(22):e012558.
12.Van D , Mcverry F , Vos J A , et al. Collateral flow predicts outcome after basilar artery occlusion: The posterior circulation collateral score.[J]. International Journal of Stroke Official Journal of the International Stroke Society, 2016:768.
13.Fahed R , Lecler A , Sabben C , et al. DWI-ASPECTS (Diffusion-Weighted Imaging–Alberta Stroke Program Early Computed Tomography Scores) and DWI-FLAIR (Diffusion-Weighted Imaging–Fluid Attenuated Inversion Recovery) Mismatch in Thrombectomy Candidates[J]. Stroke, 2017:STROKEAHA.117.019508.
14.Nakamura, Masanobu, Shigematsu, et al. Collateral circulation via the circle of Willis in patients with carotid artery steno-occlusive disease: evaluation on 3-T 4D MRA using arterial spin labelling[J]. Clinical Radiology Journal of the Royal College of Radiologists, 2015.
15.Fabritius M P ,Thierfelder K M , Meinel F G , et al. Early Imaging Prediction of Malignant Cerebellar Edema Development in Acute Ischemic Stroke.[J]. Stroke, 2017:STROKEAHA.117.018237.
16.Broocks G , Kniep H , Schramm P , et al. Patients with low Alberta Stroke Program Early CT Score (ASPECTS) but good collaterals benefit from endovascular recanalization[J]. Journal of Neurointerventional Surgery, 2019:neurintsurg-2019-015308.
17.Vagal A , Aviv R , Sucharew H , et al. Collateral Clock Is More Important Than Time Clock for Tissue Fate[J]. Stroke, 2018, 49(9):2102-2107.
18.Dargazanli C,Consoli A,Barral M,et al. Impact of modified TICI 3 versus modified TICI 2b reperfusion score to predict good outcome following endovascular therapy[J].AJNR,2017,38( 1) : 90-96.
Figures
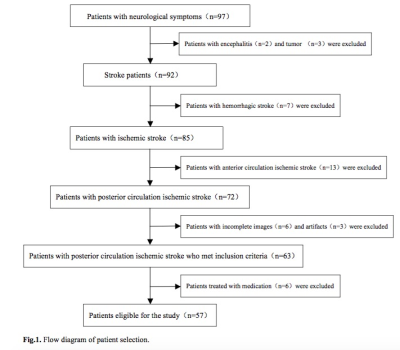
A total of 97 patients were examined; after excluding 2 patients with encephalitis, 3 patients with brain tumors, 7 patients with cerebral hemorrhage, 13 patients with anterior circulation stroke, 6 patients with incomplete baseline imaging data, 3 patients with poor image quality (artifacts), and 6 patients who met the inclusion criteria but selected drug treatment, a total of 57 patients who met the conditions and underwent mechanical thrombectomy were ultimately included (Fig.1).
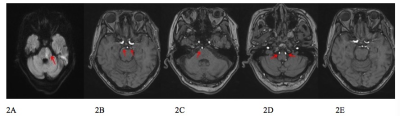
2A: DWI shows pontine infarction, DWI-pcASPECTS 8 points; Figure 2B-2E MRA original image, 2B: bilateral superior cerebellar artery development, 2C: right anterior inferior cerebellar artery development, left anterior inferior cerebellar artery not found, 2D: bilateral vertebral artery and bilateral posterior inferior cerebellar artery development, 2E: bilateral posterior communicating artery not open, MRA-collateral circulation score of 5 points. The MR-pcASCO score was 13 points, and the 90-day mRS score was 4 points. The prognosis of the patient was poor.
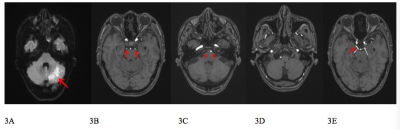
3A: DWI shows left cerebellar hemisphere infarction, DWI-pcASPECTS 9 points; 3B: bilateral superior cerebellar artery development, 3C: bilateral anterior inferior cerebellar artery development, 3D: right vertebral artery and posterior inferior cerebellar artery development, left vertebral artery and posterior inferior cerebellar artery not found, 3E: right posterior communicating artery is open, the diameter is similar to P1 segment of posterior cerebral artery, MRA-collateral circulation score of 7 points. 90-day mRS score 2 points. The prognosis of the patient was good.
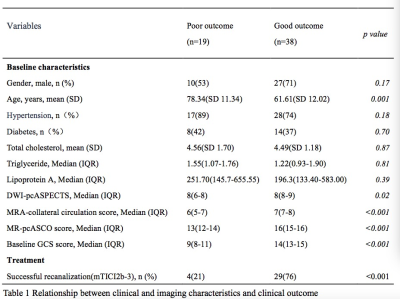
A total of 57 patients were divided into two groups according to the modified Rankin scale (mRS) at 90 days. There were 19 patients in the poor prognosis group (mRS≥3) and 38 patients in the good prognosis group (mRS≤2). There were no significant differences in sex, hypertension, diabetes, total cholesterol, triglycerides or lipoprotein A (P > 0.05). There were significant differences in age, the baseline Glasgow Coma Scale (GCS) score, the DWI-pcASPECTS, the MRA-collateral circulation score, the MR-pcASCO score and the mTICI 2B-3 (P < 0.05)
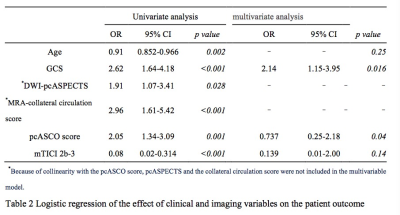
In univariate regression analysis, age, baseline GCS score, DWI-pcASPECTS, MRA-collateral circulation score, MR-pcASCO score, and mTICI 2b-3 were significantly associated with favorable clinical outcomes. In the multivariate logistic regression analysis, the baseline GCS score (OR:2.14, P =0.016) and MR-pcASCO score (OR:0.74, P =0.04) were still significantly and independently associated with good functional outcome.
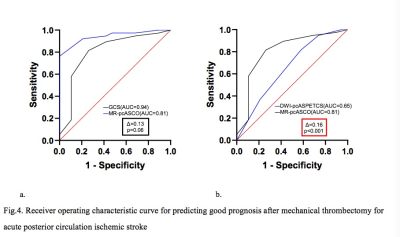
Taking the mRS at 90 days as a state variable, univariate ROC curve analysis revealed that the GCS score (AUC:0.94,95% CI: 0.89-1.00) and MR-pcASCO score (AUC:0.81,95% CI: 0.67-0.94) had higher diagnostic efficacy for prognosis, followed by the MRA- collateral circulation score (AUC:0.79,95% CI: 0.66-0.92) and DWI-pcASPECTS (AUC:0.65,95% CI: 0.50-0.81).
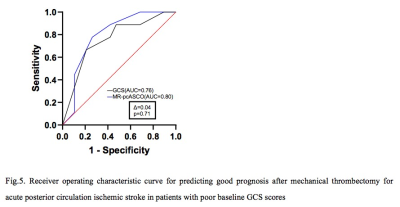
The best cutoff values for the pcASCO score and GCS score were ≥14.5(sensitivity/specificity: 81.6%, 73.7%) and ≥13.5(sensitivity/specificity: 76.3%, 100.0%), respectively. In patients with low baseline GCS scores (GCS<13.5), the diagnostic efficacy of the MR-pcASCO score (AUC:0.80, 95% CI: 0.63–0.97) was slightly higher than that of the GCS score (AUC:0.76, 95% CI: 0.56–0.95), but there was no statistically significant difference between them (P =0.71).
DOI: https://doi.org/10.58530/2023/1947