Ling Li1, Xiaoling Zhang1, Xiaoyan Lei1, Min Tang1, Xuejiao Yan1, Yu Wen1, Jing Zhang1, and Kai Ai2
1Department of MRI, Shaanxi Provincial People's Hospital, Xi’an, China, 2Philips Healthcare, Xi’an, China
Synopsis
Keywords: Vessel Wall, Atherosclerosis, ASL, transient ischemic attack
In order to prevent TIA patients from further developing into irreversible stroke, it is important to predict the occurrence of stroke in TIA patients. In this study, high-resolution magnetic resonance imaging (HRMRI) and arterial spin labeling (ASL) were used to investigate the differences of middle cerebral artery (MCA) plaque and hemodynamics in patients with ischemic stroke and TIA, and to establish a predictive model for ischemic stroke. The results showed that positive remodeling, enhancement ratio and 2.5s ATA present could be used to predict the occurrence of stroke in patients with TIA, and the prediction model had excellent diagnostic performance.
Introduction
Intracranial atherosclerotic stenosis (ICAS) is the main cause of acute ischemic stroke (AIS) or transient ischemic attack (TIA), among which middle cerebral artery (MCA) is the most commonly involved part[1-2]. The incidence of subsequent stroke in patients with TIA is high[3-4]. Therefore, how to accurately assess the occurrence of irreversible stroke is currently a major issue. The occurrence of stroke is related to the vascular lumen characteristics, plaque characteristics and cerebral blood flow defects of ICAS[5]. Previous studies used high-resolution magnetic resonance imaging (HRMRI) to characterize plaque features and dynamic sensitivity contrast-enhanced (DSC) perfusion-weighted imaging (PWI) to reflect hemodynamic injury[6]. However, as far as we know, there is no study on the combination of HRMRI and ASL to characterize the plaque features and hemodynamic changes of intracranial arterial stenosis. Different from DSC PWI, ASL can provide a simple and convenient visual assessment of arterial transport artifacts (ATA) [7-8]. Therefore, in this study, HRMRI and ASL were used to investigate the differences of MCA plaque characteristics and hemodynamics in patients with ischemic stroke and TIA, and to establish a predictive model for ischemic stroke.Materials and Methods
Consecutive patients with sICAS were retrospectively collected from October 2020 to December 2021. All patients underwent MR imaging using a 3.0 T MR scanner (Ingenia CX, Philips Healthcare, the Netherlands) with a 32-channel head coil. Imaging sequences include: T1WI, T2WI, FLAIR, DWI, TOF-MRA, black-blood pre-contrast T1WI, contrast-enhanced T1WI, and pseudo-continuous ASL [post labeling delay (PLD): 1.5s and 2.5s]. Patients were divided into TIA group and stroke group according to whether cerebral infarction occurred in MCA area on DWI. A total of 85 participants were finally evaluated with 47/38 were assigned to TIA/stroke group. Two experienced neuroradiologists blinded to any clinical information, assessed vascular lumen and plaque features at the narrowest site of the MCA on HRMRI images and assessed the presence of ATA on 2-PLD ASL images. The intraclass correlation coefficient (ICC) was used to find the inter-observer reproducibility for the measurements. Logistic regression (binary variables) analyses were performed to assess the different features between TIA and stroke group. Receiver operating characteristic (ROC) curves were used to evaluate the diagnostic performance of the different models. Z-test was used to compare the area under the curve (AUC) of each model. SPSS (version 26) or R (version 4.0.4) was used for statistical analysis. A significant difference was assumed if p < 0.05.Results
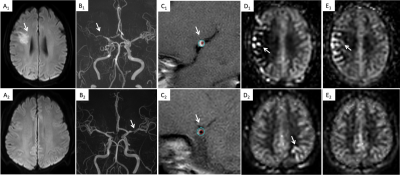
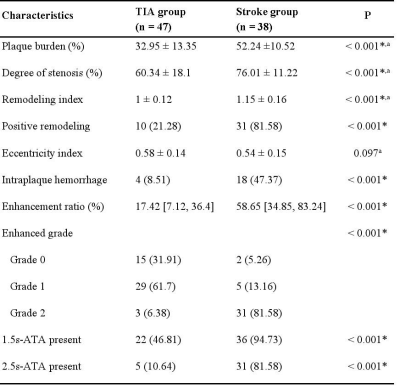
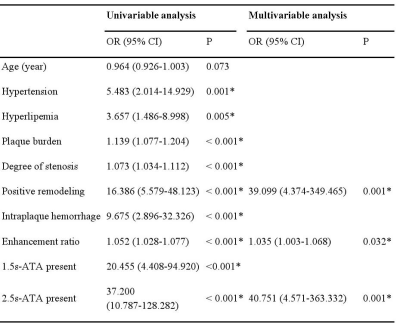
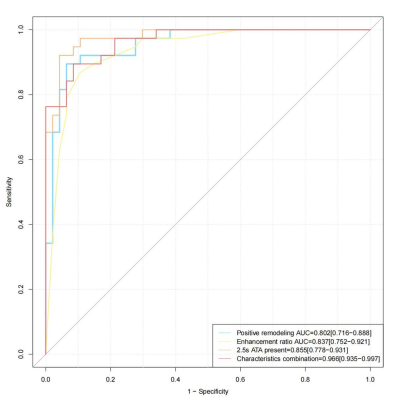
Figure 1 shown two typical example images and corresponding measurements. Compared with the TIA group, the stroke group had significantly more patients with hypertension, hyperlipidemia (Table 1). Plaque burden, degree of stenosis, enhanced ratio, prevalence of positive remodeling, intraplaque hemorrhage, 1.5s-ATA present and 2.5s-ATA present were significantly higher in stroke than those in the TIA group (Table 2). Multivariable regression analysis revealed that positive remodelling, enhancement ratio, and 2.5s-ATA present were risk factors for patients with ischemic stroke after adjusting for clinical confounding factors (both P < 0.05) (table 3). In distinguishing between patients with ischemic stroke and TIA, the diagnostic accuracy of the combination of positive remodeling, enhancement ratio, and 2.5s-ATA present was higher than that of the above single features (Figure 2). The combination had a significantly higher AUC than positive remodeling (95% CI 0.086–0.243,Z=4.089,p<0.001), enhancement ratio (95%CI 0.052–0.207,Z=3.278,p<0.001) and 2.5s-ATA present (95%CI 0.048–0.173,Z=3.482,p<0.001), respectively. The combination of three characteristics had a sensitivity of 89.47%, a specificity of 91.49%, a positive predictive value of 89.47%, a negative predictive value of 91.49%, and an accuracy of 90.59% .Discussion
This study found that the plaque characteristics of positive remodeling was significantly higher in stroke group than that in TIA group. While positive remodeling is associated with high-risk plaques, our results suggest that plaque instability may be higher in stroke patients than in TIA patients. In addition, enhancement ratio was much higher in stroke group. As plaque enhancement is related to neovascularization, inflammation, and endothelial dysfunction leading to leakage of gadolinium, the higher the enhancement ratio, the more severe the endothelial dysfunction and the greater the possibility of irreversible stroke is. The results of a recent meta-analysis showed plaque enhancement, positive wall remodeling are significantly associated with downstream ischemia. These plaque features may contribute to the abnormal distal blood flow, allowing ATA effect in the stroke group even when PLD was 2.5s. Therefore, the prolongation of PLD increases the difference of blood flow abnormalities between TIA patients and stroke patients. ASL with multi-PLD has more clinical value than the ASL with single PLD in intracranial stenosis evaluation.Conclusion
We have demonstrated that positive remodelling, enhancement ratio, and 2.5s-ATA present are more strongly associated with ischemic stroke than with TIA. Moreover, we have developed a predictive model for subsequent irreversible stroke in patients with TIA. Our work provides a scientific basis for early risk stratification and early clinical intervention in patients with TIA. Acknowledgements
No acknowledgement foundReferences
[1] Chen PH,Gao S,Wang YJ,et al.Classifying Ischemic Stroke, from TOAST to CISS.CNS Neurosci Ther. 2012;18(6): 452–456.
[2] Wong KS, Li H.Long-term mortality and recurrent stroke risk among Chinese stroke patients with predominant intracranial atherosclerosis. Stroke. 2003;34(10): 2361-6.
[3] Garg A, Limaye K, Shaban A,et al.Risk of Ischemic Stroke after an Inpatient Hospitalization for Transient Ischemic Attack in the United States.NEUROEPIDEMIOLOGY. 2021-01-01;55(1):40-46.
[4] Mendelson, SJ; Prabhakaran, S. Diagnosis and Management of Transient Ischemic Attack and Acute Ischemic Stroke.JAMA-J AM MED ASSOC. 2021-03-16;325(11):1088-1098.
[5] Liu S, Luo Y, Wang C, et al. Combination of plaque haracteristics, pial collaterals, and hypertension contributes to misery perfusion in patients with symptomatic middle cerebral artery stenosis. J Magn Reson Imaging.2020;51:195–204.
[6] Liu S , Tang R , Xie W, et al. Plaque characteristics and hemodynamics contribute to neurological impairment in patients with ischemic stroke and transient ischemic attack.[J]. European radiology. 2021;31(4):2062-2072.
[7] Zaharchuk G. Arterial spin-labeled perfusion imaging in acute ischemic stroke. Stroke. 2014;45(4):1202–1207.
[8] Bang OY, Goyal M, Liebeskind DS. Collateral circulation in ischemic stroke: assessment tools and therapeutic strategies. Stroke. 2015;46(11):3302–3309.