1925
3 T MR Neuroimagingand CT Guided Injection for Atypical Facial Pain: A multimodality analysis of Pain Response1Affiliated Hospital of North Sichuan Medical College, Nanchong 637000, Nanchong, China, 2The Fifth People's Hospital of Chengdu, Chengdu, China, 3Second Affiliated Hospital of North Sichuan Medical College,Nanchong 637100, Nanchong, China, 4MR Scientific Marketing, Siemens Healthcare, Shanghai, China, Shanghai, China
Synopsis
Keywords: Neurodegeneration, Neurodegeneration
At present, the pathogenesis of atypical facial pain is unknown. We conducted pain related analysis on the included patients through magnetic resonance imaging and trigeminal neurolysis, and the results suggest that trigeminal neuropathy may be a pathogenesis of atypical facial pain.Introduction
Atypical facial pain (AFP) or currently called persistent idiopathic facial pain (PIFP) is an idiopathic facial pain. Although the pain area is similar to trigeminal neuralgia, AFP usually shows persistent facial pain without the characteristics of cranial neuralgia [1]. AFP patients often show persistent burning sensation and dull pain on one side, often accompanied by a certain degree of depression and anxiety [2-4]. At present, there is no uniform standard for the treatment of AFP, and there is no expert consensus and international guidelines in this field [5]. Magnetic resonance neuroimaging (MRN) is increasingly used in peripheral neuropathy diagnosis and treatment of changes [6-9] . This high-resolution imaging mode can localization of trigeminal neuropathy is reported to be useful for guiding therapeutic injections and surgery interventions[10]. MRN findings include signal changes, space occupying, vascular nerve compression, etc., especially the high signal changes of the affected trigeminal nerve. Localization of neuropathy on MRN is possible because signal changes and/or aperture changes on MRI weighted images are most pronounced at the affected site. In this article, we evaluated the effect of CT-guided injection therapy in patients with normal/abnormal signals on MRN, which is reported as follows.Methods
A retrospective cross-sectional evaluation of this study was carried out, which was approved by the Ethics Committee of the Affiliated Hospital of North Sichuan Medical College, and all patients signed informed consent forms. A total of 91 patients were included in the study, and there were 139 CT-guided trigeminal neurolysis. All patients received CT-guided trigeminal neurolysis. All patients underwent MRN imaging of trigeminal nerve on a 3T MR scanner(MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). All patients had preoperative MR trigeminal neuroimaging.The scanning parameters are as follows Table 1.The image results were collected and analyzed by two senior radiologists. The main data collected include: demographic data (age, sex); Chief complaint; Initial symptoms; Operation date and MRN imaging results; Pain score before and after injection; Number of days to relieve pain; The quality of pain, quality of life and pain scores reported by patients during follow-up improved; complication; And whether any other surgery was performed to relieve the pain. The response to CT guided trigeminal neurolysis was divided into three groups: positive, possibly positive and negative. CT guided peripheral trigeminal neurolysis was regarded as positive, and the "must meet" criteria were: 1) pain score decreased by at least 50% in the first 24 hours; 2) The reaction lasted for 24 hours and 48 hours, that is, after the initial decrease to less than 50%, the pain no longer increased to more than 50%. When the pain score decreases by less than 2 points, the result will be considered as negative. Those who were considered as possible positive block showed some benefits to patients without meeting the strict criteria for positive block. This includes patients reporting injection time for more than 24 hours of pain relief delay, patients reporting a pain score decrease of less than 50% but more than 2 points, and patients reporting a significant pain score decrease that did not last until the 48 hour time point. Statistical analysis: A crosstab was generated to compare the correlation between MRN results and improvement in pain scores. The improvement score of pain score is 0=no improvement, 1=possible improvement or 2=confirmed improvement. The chi square test is used to test any correlation, and the Cochran Armit age trend test is used to test any trend. The significance level was set at 0.05. All analyses were completed in SPSS 23.0 statistical software (SPSS, Chicago, IL).RESULTS
A total of 91 patients were included in the study, with an age range of 21 to 93 years (mean = 52.3 years, standard deviation (SD) = 11.2 years) and a male to female ratio of 1:1.8. The most common complaint was persistent pain and discomfort on one side of the face (86 / 91). Forty-eight of 91 patients underwent two neurolysis. In MRN imaging of 91 patients, 62 patients showed trigeminal nerve changes, and 29 patients were negative. There were 32 cases of vascular nerve compression and 30 cases of abnormal nerve signal. Among the cases with abnormal nerve signals, 22 cases had abnormal maxillary nerves and 8 cases had abnormal mandibular nerves.Of the CT-guided lysis therapy, out of 139 trigeminal lysis, 41 were positive (29.5%), 52 were likely positive (37.4%), and 46 were negative (33.1%). In these groups, the percentage of positive and negative MRN results are listed in Table 1. In MRN positive and negative cases, the treatment rate of CT-guided release is listed in Table 2.Discussion
In our study, MRN results showed that 68.1% of atypical facial pain patients showed trigeminal nerve abnormalities, which may indicate that atypical facial pain may be a subtype of trigeminal neuralgia. Among these abnormal manifestations, the most common is vascular nerve compression, followed by abnormal signal changes. Among them, the maxillary nerve and mandibular nerve were mainly changed, and no abnormality of ophthalmic nerve signal was found. This is also consistent with the clinical symptoms, because most of the symptoms of atypical facial pain are limited to the second and third branches. The preoperative neuroimaging examination of the trigeminal nervous system can help us understand the potential pathogenic factors of atypical facial pain, including trigeminal neurovascular compression or neurodegenerative changes and degeneration. In MRN positive cases, the effect of CT guided neurolysis was significantly higher than that of negative cases, while in some negative cases, whicn also achieved therapeutic effect, which made us clearly aware that the potential pathogenesis of atypical facial pain still needs to be further exploredConclusion
MRN of atypical facial pain suggests that atypical facial pain may be caused by trigeminal neuropathy. However, some patients with negative MRI findings cannot completely rule out the possibility of trigeminal neuropathy, which needs further study.Acknowledgements
The authors would like to thank Dr. Anup Bhetuwal for revising the article.
References
1. Forssell Heli, Tenovuo Olli, Pekka Silvoniemi, et al. Differences and similarities between atypical facial pain and trigeminal neuropathic pain.Neurology. 2007 Oct 02;69(14):1451-9.
2. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition.Cephalalgia : an international journal of headache.2018;38(1)1-211.
3. Nguyen, Chau T, Wang, Marilene B. Complementary and integrative treatments: atypical facial pain. Otolaryngol Clin North Am.2013V46N3:367-82.
4. Krolczyk SJ, Kalidas K, Myers MA. Persistent idiopathic facial pain. 2010. Available at: http://emedicine. medscape.com/article/1142187-overview. Accessed January 11, 2012.
5. Rahimpour, Shervin, Lad, Shivanand P. Surgical Options for Atypical Facial Pain Syndromes. Neurosurg Clin N Am.2016V27N3:365-70.
6. Delaney H, Bencardino J, Rosenberg ZS. Magnetic resonance neurography of the pelvis and lumbosacral plexus. Neuroimaging Clin N Am 2014; 24:127- 150.
7. Pham M, Baumer T, Bendszus M. Peripheral nerves and plexus: Imaging by MR-neurography and high-resolution ultrasound. Curr Opin Neurol 2014; 27:370-379.
8. Fisher S, Wadhwa V, Manthuruthil C, Cheng J, Chhabra A. Clinical impact of magnetic resonance neurography in patients with brachial plexus neuropathies. Br J Radiol 2016; 89:20160503.
9. Soldatos T, Andreisek G, Thawait GK, Guggenberger R, Williams EH, Carrino JA, Chhabra A. Highresolution 3-T MR neurography of the lumbosacral plexus. Radiographics 2013; 33:967-987.
10. Wadhwa V, Hamid AS, Kumar Y, Scott KM, Chhabra A. Pudendal nerve and branch neuropathy: Magnetic resonance neurography evaluation. Acta Ra-diol 2017; 58:726-733
Figures
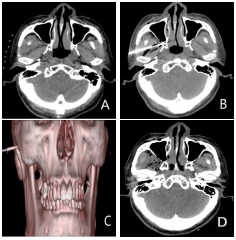
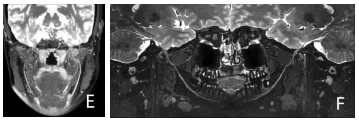
Figure 2. A 46-year-old female with persistent pain in the left face and mandible for half a year, VAS score was 6 points, MRN showed that the signal of left mandibular nerve increased, suggesting that neuritis might change; Figure F. A 41-year-old male with persistent facial and mandibular pain for 8 months, VAS score was 7 points, MRN showed thickening of the right mandibular nerve and increased signal intensity.
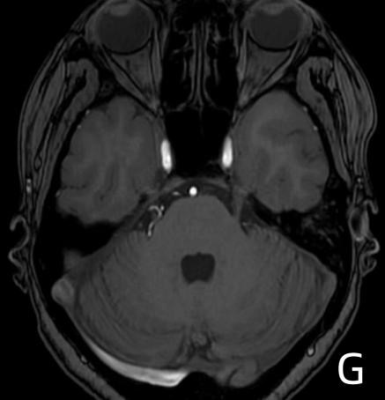
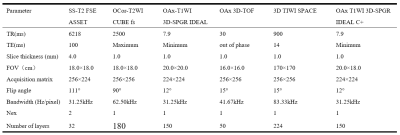
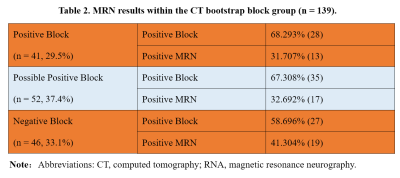
Table 2. MRN results within the CT bootstrap block group (n = 139).
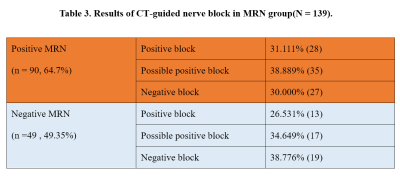
Table 3. Results of CT-guided nerve block in MRN group(N = 139).