1917
End-of-life symptoms and imaging signs in COVID-19 patients with renal failure induced encephalopathy1Radiology, NYU Grossman School of Medicine, New York, NY, United States
Synopsis
Keywords: Neuroinflammation, Toxicity, Encephalopathy, COVID, renal, toxic
COVID-19 continues to be a threat to global public health. A large number of studies have reported various neurological symptoms in COVID-19 patients even after the respiratory symptoms have resolved. In severe cases, the neurological complications induced by SARS-CoV-2 can lead to extensive neuroimaging abnormality. Additionally, previous studies have shown that, among COVID-19 patients who went through dialysis, the short-term mortality rate is high. In this study, we reported three cases of deceased patients who had severe encephalopathy while going through dialysis, to better understand their fatal disease course and associated brain MRI and clinical symptoms complicated by COVID-19.INTRODUCTION
COVID-19 continues to be a threat to global public health and has claimed the lives of over one million people in the United States. A large number of studies have reported various neurological symptoms in COVID-19 patients even after the respiratory symptoms have resolved. In severe cases, the neurological complications induced by SARS-CoV-2 can lead to extensive neuroimaging abnormalities. Additionally, previous studies have shown that, among COVID-19 patients who went through dialysis, the short-term mortality rate is high. In this study, we reported three cases of deceased patients who had severe encephalopathy while going through dialysis, to better understand their fatal disease course and associated brain MRI and clinical symptoms complicated by COVID-19.CASE REPORTS
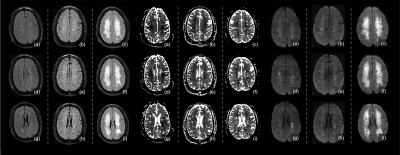
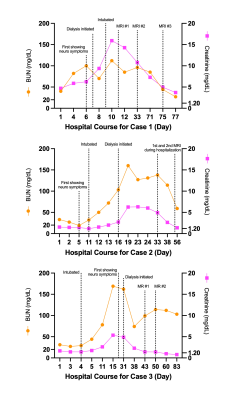
[Case#1]A 48-year-old male patient with a history of hypertension, hyperlipidemia, chronic kidney disease, and obesity. At admission, the patient presented with cough and myalgia for one week. He had endorsed diarrhea, fever, nausea, vomits, and abdominal pain. He was found to be positive for COVID-19 and his lab test showed high values for BUN 40 and Cr 4.71. With the development of acute kidney injury, the patient started dialysis on day 7 of admission and began to have delayed verbal and motor response. On day 9, his chest X-Ray showed worsening patchy areas and thus he was intubated due to shortness of breath. The CT result showed likely encephalopathy on the same day. The patient went through the first brain MR imaging on day 11, showing multiple new strokes in the watershed areas, as well as new scattered white matter hyperintensities (WMHs) (Figure 1). Three weeks later, the patient’s mental status worsened, with the second MR imaging on day 33 showing more areas with patchy and confluent hyperintensities on T2 FLAIR that have restricted diffusion on ADC map (Figure 1). Five weeks later, on day 75 of admission, he appeared to be in a vegetative state. The third MRI showed profound changes and drastic progression, showing significantly increased confluent areas that became diffuse and worsened diffusion restriction (Figure 1). Despite his improved lab results after dialysis, his lung volume remained low as seen in the chest X-Ray, and no sign of mental status improvement was observed. The patient died six weeks after that.
[Case#2]
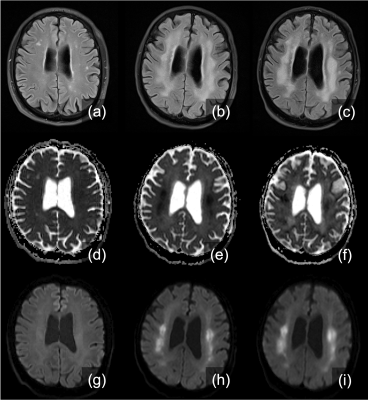
A 73-year-old male patient with a history of coronary artery disease, Crohn’s disease, spinal stenosis, and prostate cancer with mets. He had had cough, nauseas, and back pain for unknown number of days. At admission, he had fever and acute hypoxic respiratory failure. Chest X-Ray showed atypical pneumonia and was confirmed to be COVID positive. His oxygen demands increased, and he was intubated on day 11. His condition was later complicated by atrial fibrillation, gastrointestinal bleed requiring blood transfusions. With his renal function deteriorating, hemodialysis was initiated on day 16. The brain MRI scan on day 33 showed extensive and confluent bilateral FLAIR hyperintensity, which was unseen compared to the scan 6 years prior (Figure 3). Although his lab test result improved, he was in a minimally conscious or vegetative state, with his second MRI showing worsening results (Figure 3). Four days later, the patient’s wife decided to remove ventilator support. Patient died two days after that.
[Case#3]
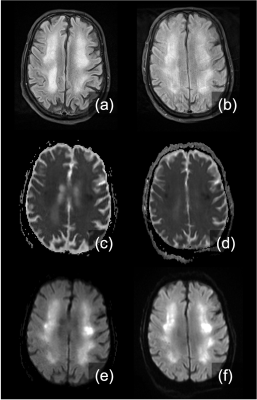
A 73-year-old male patient with a history of hypertension, hyperlipidemia, and chronic kidney disease. He tested positive for COVID two weeks before admission but was asymptomatic. One week prior to admission, he developed worsening fatigue and decreased appetite. On the day of admission, his family members noticed his lethargic behaviors, and tested for oxygen level. He was later admitted to the hospital due to low oxygen level (around 70%) and positive COVID test. At admission, he had no respiratory distress, cough, or shortness of breath. His hypoxia worsened quickly, and he was intubated on day 4, with chest X-Ray showing worsening multifocal airspace opacities compared to initial radiographs. He later developed pneumothorax and underwent tracheostomy twice. His renal function also deteriorated quickly, and hemodialysis was initiated on day 31 (BUN 162, Cr 4.88). He had been presenting altered mental status for a week. The first brain MRI on day 43 (Figure 4) showed confluent hyperintensities in FLAIR, which were seen again on the second MRI scan one week later (Figure 4). His renal function was partially recovered after dialysis, while the encephalopathy did not improve. His respiratory and neurological conditions did not improve, and his course was later complicated by sepsis. He died due to a cardiopulmonary arrest on day 94.
DISCUSSION AND CONCLUSION
The reported three severe COVID cases here a larger cohort with typical pattern of disease progression on MRI including acute and progressive encephalopathy with water restriction (hypointense on ADC, hyperintense on TRACE imaging) and patchy and confluent lesions in white matter. Besides the most common manifestation of ARDS, the disease progression within this cohort is also complicated by pre-existing health conditions and development of acute kidney injury. Their neurological symptoms and neuro-imaging findings also showed similar patterns. Renal failure seemed to contribute to the initial brain damage and worsening of neurological conditions despite the improved blood BUN and creatinine levels (Figure 2) after dialysis, all three cases ended up in a vegetative state.Acknowledgements
References
1. Frontera, Jennifer A., et al. "Toxic metabolic encephalopathy in hospitalized patients with COVID-19." Neurocritical care 35.3 (2021): 693-706.
2. Soltani Zangbar, Hamid, Ali Gorji, and Tahereh Ghadiri. "A review on the neurological manifestations of COVID-19 infection: a mechanistic view." Molecular neurobiology 58.2 (2021): 536-549.
3. Hemmelder, Marc H., et al. "Recovery of dialysis patients with COVID-19: health outcomes 3 months after diagnosis in ERACODA." Nephrology Dialysis Transplantation 37.6 (2022): 1140-1151.APA
4. Bauer, Lisa, et al. "The neuroinvasiveness, neurotropism, and neurovirulence of SARS-CoV-2." Trends in Neurosciences (2022).
5. Umapathi, Thirugnanam, et al. "Encephalopathy in COVID-19 patients; viral, parainfectious, or both?." Eneurologicalsci 21 (2020): 100275.APA
6. Ahmed, Manzoor, et al. "COVID-Related Leukoencephalopathy: Unusual MRI Features and Comparability to Delayed Post Hypoxic Ischemic Encephalopathy." Radiology Case Reports 17.3 (2022): 852-855.APA
7. Koralnik, Igor J., and Kenneth L. Tyler. "COVID‐19: a global threat to the nervous system." Annals of neurology 88.1 (2020): 1-11.
8. Kremer, Stéphane, et al. "Brain MRI findings in severe COVID-19: a retrospective observational study." Radiology 297.2 (2020): E242-E251.
Figures