1907
Cardiovascular Magnetic Resonance Imaging Appearance During the Acute, Intermediate and Convalescent Phase of COVID-19 Patient1Shanghai Jiao Tong University School of Medicine Affiliated Renji Hospital, Shanghai, China, 2Philips Healthcare, Shanghai, China, 3Beijing Anzhen Hospital, Capital Medical University, Shanghai, China
Synopsis
Keywords: Heart, COVID-19, review
The purpose is to find the cardiac involvement features of COVID-19 using cardiac MRI, and set forth the relationship of these cardiac features with their clinical presentation. We analyzed the results under the separate cardiovascular magnetic resonance sequences combining different stages, as well as consider the unique conditions when cardiovascular signs and symptoms are present.Introduction
Progressively more studies demonstrate that COVID-19 affects the cardiovascular system. The symptoms of palpitation, arrhythmia, pericardial effusion, myocarditis, myocardial infarction,1 and even sudden death as a result of cardiac involvement2 may be clearly present. Cardiovascular magnetic resonance (CMR) has particular value for patients with COVID-19, for that CMR imaging has been used to identify changes in the structure and function of the heart which can be observed quantitatively and qualitatively with high sensitivity.3,4 The purpose of this review focuses on the cardiac features of COVID-19 patients using CMR during the course of disease: the acute phase, the recovery phase, and the Intermediate phase that bridging the two phases mentioned above, and set forth the relationship of these cardiac features with their clinical presentation.Methods
The relevant literatures were analyzed according to different sequences. Cardiac cine imaging is one way to analyze myocardial anatomy and function. 5 Late gadolinium enhancement (LGE) images identify fibrosis or infarction.6 In T2-weighted imaging, edema can be identified.7 However, frequent breath holding5 and arrhythmias7 can pose imaging problems in the form of artifacts, which reduces the accuracy. T2 short tau inversion recovery (T2-STIR) sequence can better identify edema.8 In the Global longitudinal strain (GLS) analysis, abnormal GLS is suggestive of early mechanical dysfunction of the heart.9 T1 mapping, T2 mapping, and extracellular volume (ECV) can depict diffuse fibrosis or inflammation processes.6Results
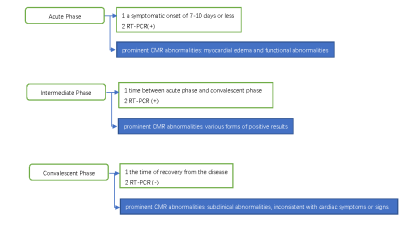
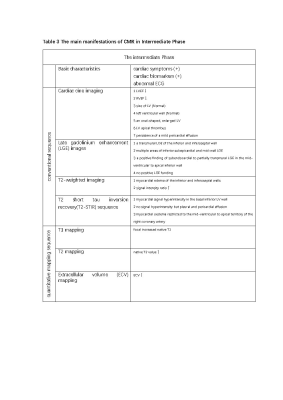
In order to compare the diverse cardiac presentation seen throughout the progression of COVID-19, we propose a concise classification dividing the course of disease into three periods. Figure 1 demonstrates the classification and general Characteristics. The acute phase refers to a symptomatic onset of 7-10 days or less, and patients are confirmed to have SARS-CoV-2 infection by reverse transcription-polymerase chain reaction (RT-PCR). In this phase, irreversible injury such as necrosis or replacement myocardial fibrosis is not infrequent.10, 11 In some cases, cardiac injury is the sole manifestation of COVID-19 infection, without the presence of pneumonia.12, 13 Table 1 summarizes the main manifestations in acute phase. The recovery phase refers to the time of recovery from the disease as well as a confirmed negative result on RT-PCR[LW1] . In this phase, there are subclinical myocardial abnormalities,14 even in patients with no preexisting cardiovascular disease or symptoms.15 Table 2 summarizes the main manifestations in recovery phase. The third phase is the bridge between the two periods. In this phase, a thrombotic state can be detected in some cases.16, 17 Furthermore, cardiac injury is strongly related to specific laboratory biomarkers, and a linear relationship has been established between the two.18, 19 Table 3 summarizes the main manifestations in this phase.Discussion
Acute PhaseAbnormal motion and low ventricular ejection fraction can be easily identified. LGE findings are not commonly seen during this phase. When there is a positive finding, in many cases it is limited to a relatively minute area usually in the sub-epicardium . Hyperemia and edema are common, always involving a relatively large area of heart. GLS further reduced in patients with higher cardiac biomarkers. elevated T1 values, T2 and ECV values are typically detected, positively correlated with cardiac biomarkers. 10,11,12,13,20,21
Convalescent Phase
The size and function of either ventricle is frequently within normal range during this phase, which may seem inconsistent with the abnormal clinical signs or symptoms. LGE closely corresponds with cardiac symptoms and biomarkers, which are typically found in the subepicardium. Edema is less reported during this period, positive findings are correlated with cardiac symptoms and cardiac enzyme levels. a reduced GLS can be observed in subclinical abnormalities. Increased T1, T2 values can usually be found in patients with cardiac symptoms and abnormal cardiac biomarkers. Elevated ECV can be detected, even if there are no discernible cardiac symptoms or abnormal cardiac biomarkers. 14,15,22,23,24,25,26,27,28
Intermediate Phase
Regional wall motion abnormalities and impaired LV systolic function during this phase are more distinguishable There may also be LV dilation, ventricular aneurysm, or mild pericardial effusion. Cardiac injury from COVID-19 progresses slower than the symptomatic presentation and is easier to detect during the intermediate. LGE can be found in the sub-epicardium and septal mid0wall, or the transmural sub0endocardium. Positive LGE findings in most people are associated with abnormal signs and symptoms, with the exception of pregnant women. This is likely related to the anatomic and physiologic changes that occur during this time, in particular the immunologic modifications leading to maternal tolerance of the allogenic fetus.29 Myocardial edema is reported in certain cases, tending to be localized edema, with occasional pericardial effusion. Focal increased native T1 can be seen. T2 values and ECV are related to abnormal cardiac symptoms and signs. 16,17,18,19,30
Conclusion
Cardiac involvement caused by COVID-19 can occur at any stage. Early cardiac involvement tends to be acute inflammation or infarction. The cardiac involvements during the convalescent period are generally mild, while during the intermediate phase are often obvious, serious and diverse.Acknowledgements
We are very grateful to the Philips Healthcare team for their support in image analysis.References
1. Dhakal BP, Sweitzer NK, Indik JH, Acharya D, William P. SARS-CoV-2 Infection and Cardiovascular Disease: COVID-19 Heart. Heart, lung & circulation 2020;29(7):973-987.
2. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive care medicine 2020;46(5):846-848.
3. Motwani M, Kidambi A, Greenwood JP, Plein S. Advances in cardiovascular magnetic resonance in ischaemic heart disease and non-ischaemic cardiomyopathies. Heart (British Cardiac Society) 2014;100(21):1722-1733.
4. Han Y, Chen Y, Ferrari VA. Contemporary Application of Cardiovascular Magnetic Resonance Imaging. Annual review of medicine 2020;71:221-234.
5. Göransson C, Ahtarovski KA, Kyhl K, Lønborg J, Nepper-Christensen L, Bertelsen L, Ghotbi AA, Schoos MM, Køber L, Høfsten D, Helqvist S, Kelbæk H, Engstrøm T, Vejlstrup N. Assessment of the myocardial area at risk: comparing T2-weighted cardiovascular magnetic resonance imaging with contrast-enhanced cine (CE-SSFP) imaging-a DANAMI3 substudy. European heart journal. Cardiovascular Imaging 2019;20(3):361-366.
6. Russo V, Lovato L, Ligabue G. Cardiac MRI: technical basis. La Radiologia medica 2020;125(11):1040-1055.
7. Abdel-Aty H, Simonetti O, Friedrich MG. T2-weighted cardiovascular magnetic resonance imaging. Journal of magnetic resonance imaging : JMRI 2007;26(3):452-459.
8. Francone M, Carbone I, Agati L, Bucciarelli Ducci C, Mangia M, Iacucci I, Catalano C, Passariello R. Utility of T2-weighted short-tau inversion recovery (STIR) sequences in cardiac MRI: an overview of clinical applications in ischaemic and non-ischaemic heart disease. La Radiologia medica 2011;116(1):32-46.
9. Vijapurapu R, Nordin S, Baig S, Liu B, Rosmini S, Augusto J, Tchan M, Hughes DA, Geberhiwot T, Moon JC, Steeds RP, Kozor R. Global longitudinal strain, myocardial storage and hypertrophy in Fabry disease. Heart (British Cardiac Society) 2019;105(6):470-476.
10. Blondiaux E, Parisot P, Redheuil A, Tzaroukian L, Levy Y, Sileo C, Schnuriger A, Lorrot M, Guedj R, Ducou le Pointe H. Cardiac MRI in Children with Multisystem Inflammatory Syndrome Associated with COVID-19. Radiology 2020;297(3):E283-e288.
11. Chen BH, Shi NN, Wu CW, An DA, Shi YX, Wesemann LD, Hu J, Xu JR, Shan F, Wu LM. Early cardiac involvement in patients with acute COVID-19 infection identified by multiparametric cardiovascular magnetic resonance imaging. Eur Heart J Cardiovasc Imaging 2021.
12. Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 2020;5(7):819-824.
13. Fischer Q, Brillat-Savarin N, Ducrocq G, Ou P. Case report of an isolated myocarditis due to COVID-19 infection in a paediatric patient. Eur Heart J Case Rep 2020;4(Fi1):1-5.
14. Li X, Wang H, Zhao R, Wang T, Zhu Y, Qian Y, Liu B, Yu Y, Han Y. Elevated Extracellular Volume Fraction and Reduced Global Longitudinal Strains in Patients Recovered from COVID-19 without Clinical Cardiac Findings. Radiology 2021:203998. 15. Pan C, Zhang Z, Luo L, Wu W, Jia T, Lu L, Liu WV, Qin Y, Hu F, Ding X, Qin P, Qian L, Chen J, Li S. Cardiac T1 and T2 Mapping Showed Myocardial Involvement in Recovered COVID-19 Patients Initially Considered Devoid of Cardiac Damage. J Magn Reson Imaging 2021.
16. De Vita S, Ippolito S, Caracciolo MM, Barosi A. Peripartum cardiomyopathy in a COVID-19-infected woman: differential diagnosis with acute myocarditis-A case report from a Hub Institution during the COVID-19 outbreak. Echocardiography 2020;37(10):1673-1677.
17. Burkert FR, Niederreiter L, Dichtl W, Mayr A, Virgolini I, Klauser A, Weiss G, Bellmann-Weiler R. Case report of a COVID-19-associated myocardial infarction with no obstructive coronary arteries: the mystery of the phantom embolus or local endothelitis. Eur Heart J Case Rep 2021;5(2):ytaa521.
18. Galea N, Marchitelli L, Pambianchi G, Catapano F, Cundari G, Birtolo LI, Maestrini V, Mancone M, Fedele F, Catalano C, Francone M. T2-mapping increase is the prevalent imaging biomarker of myocardial involvement in active COVID-19: a Cardiovascular Magnetic Resonance study. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance 2021;23(1):68.
19. Jin L, Tang W, Song L, Luo L, Zhou Z, Fan X, Zhang J, Wu N, Liu K, Chen J. Acute cardiac injury in adult hospitalized COVID-19 patients in Zhuhai, China. Cardiovasc Diagn Ther 2020;10(5):1303-1312. 20. Ford JS, Holmes JF, Jones RF. Cardioembolic Stroke in a Patient with Coronavirus Disease of 2019 (COVID-19) Myocarditis: A Case Report. Clin Pract Cases Emerg Med 2020;4(3):332-335.
21. Bhansali S, Minocha P, Phoon C, Henry G, Chakravarti S, Ramirez M, Bhatla P. Cardiac involvement in a pediatric patient with COVID-19: Looking beyond the nonspecific global cardiac injury. Echocardiography 2020;37(9):1488-1491.
22. Sardari A, Tabarsi P, Borhany H, Mohiaddin R, Houshmand G. Myocarditis detected after COVID-19 recovery. Eur Heart J Cardiovasc Imaging 2021;22(1):131-132.
23. Jagia P, Ojha V, Naik N, Sharma S. Myocardial fibrosis detected by cardiovascular magnetic resonance in absence of myocardial oedema in a patient recovered from COVID-19. BMJ Case Rep 2020;13(12).
24. Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, Liu W, Zeng H, Tao Q, Xia L. Cardiac Involvement in Patients Recovered From COVID-2019 Identified Using Magnetic Resonance Imaging. JACC Cardiovasc Imaging 2020 13(11):2330-2339.
25. Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur Heart J 2005;26(15):1461-74.
26. Rajpal S, Tong MS, Borchers J, Zareba KM, Obarski TP, Simonetti OP, Daniels CJ. Cardiovascular Magnetic Resonance Findings in Competitive Athletes Recovering From COVID-19 Infection. JAMA Cardiol 2021;6(1):116-118.
27. Beşler MS, Arslan H. Acute myocarditis associated with COVID-19 infection. Am J Emerg Med 2020;38(11):2489.e1-2489.e2.
28. Tschöpe C, Sherif M, Anker MS, Geisel D, Kuehne T, Kelle S. COVID-19-convalescence phase unmasks a silent myocardial infarction due to coronary plaque rupture. ESC heart failure 2021;8(2):971-973.
29. Abu-Raya B, Michalski C, Sadarangani M, Lavoie PM. Maternal Immunological Adaptation During Normal Pregnancy. Front Immunol 2020;11:575197.
30. Labani A, Germain P, Douchet MP, Beghi M, Von Hunolstein JJ, Zeyons F, Roy C, El Ghannudi S. Acute Myopericarditis in a Patient With Mild SARS-CoV-2 Respiratory Infection. CJC Open 2020;2(5):435-437.
Figures