1904
MRI for characterization of cardiac function in suspected myocarditis as post-acute sequelae of COVID-19
El-Sayed H. Ibrahim1, Jason Rubenstein1, Antonio Sosa1, Kevin Koch1, Jadranka Stojanovska2, and Ivor Benjamin1
1Medical College of Wisconsin, Milwaukee, WI, United States, 2New York University, New York, NY, United States
1Medical College of Wisconsin, Milwaukee, WI, United States, 2New York University, New York, NY, United States
Synopsis
Keywords: Myocardium, COVID-19
Among COVID-19 induced cardiac complications, myocarditis has clinical significance because it can result in permanent myocardial damage which leads to poor outcome. In this study, we studied 65 consecutive COVID-19 patients who underwent cardiac MRI post COVID-19 due to concerns of post-COVID myocarditis or other cardiomyopathies, where MRI was used to identify suspected versus excluded myocarditis based on LGE and T1/ECV/T2 mappings. The results demonstrated the value of MRI systolic strain and diastolic strain rate as sensitive markers for early detection of subclinical cardiac dysfunction and characterizing the heart contractility pattern in high-risk patients with suspected myocarditis versus excluded myocarditis.Introduction
COVID-19 has now been established to be a multisystem disease, affecting different organs of the human body. Cardiac symptoms are increasingly recognized as late complications of COVID-19 infection, even in healthy individuals with mild initial illness1. A recent study2 suggested that COVID-19 might be responsible for a sustained subacute or chronic inflammatory state of the myocardium. Among COVID-19 induced cardiac complications, myocarditis has clinical significance3 because myocardial inflammation can result in permanent myocardial damage and contribute to the development of long-term cardiac sequelae, including arrhythmia, heart failure, and sudden cardiac death. The goal of this study was to assess the value of cardiac MRI strain and strain rate parameters as sensitive markers for identifying high-risk patients with suspected post-acute myocarditis in COVID-19.Methods
In this study, we included 65 consecutive COVID-19 patients (28 males, age = 47±17 y.o.) who underwent cardiac MRI post COVID-19 (duration between diagnosis and MRI = 159±129 days) due to concern of post-COVID myocarditis (group 1; n=22) or other cardiomyopathies (group 2; n=43) based on clinical examination, symptoms, and lab results. Patients were scanned on Siemens 3T (n=49) and 1.5T (n=16) MRI scanners. The results of the MRI exams categorized the subjects as either having ‘suspected’ or ‘excluded’ myocarditis based on late gadolinium enhancement (LGE) pattern and/or elevated T1/T2/extracellular volume (ECV) parameters4. Further analysis was conducted on the cine images using the tissue tracking technique to generate global longitudinal, circumferential, and radial peak systolic strains (GLS, GCS, GRS) and global longitudinal, circumferential, and radial peak diastolic strain rates (GLSR, GCSR, GRSR). Serum hsTn (Troponin), NT proBNP, and/or hsCRP measurements were available in 60 patients (reference normal values for these parameters are ≤10 ng/L, ≤449 pg/ml, and ≤3 mg/L, respectively, based on the analysis lab). Statistical analysis was conducted to examine the significance of the differences between the suspected and excluded myocarditis groups, where P<0.05 was considered statistically significant.Results
The resulting measurements are summarized in Table 1. Suspected myocarditis based on MRI was raised in 16 patients (the ‘suspected myocarditis’ group), while myocarditis was excluded in the rest of the patients (the ‘excluded myocarditis’ group, which included 49 patients). The serum biomarkers showed a wide range of measurements within each of the studied groups, which resulted in insignificant differences between suspected and excluded myocarditis; however, average hsTn and NT proBNP measurements were larger in the suspected myocarditis group compared to the excluded myocarditis group. LVEF in the suspected myocarditis group was significantly smaller than that in the excluded myocarditis group (Table 1). On the other hand, both end-diastolic volume (EDV) and end-systolic volume (ESV) in suspected myocarditis were larger than those in excluded myocarditis. Similarly, LV mass in suspected myocarditis was larger than that in excluded myocarditis. In the right ventricle, the patterns of change in the EF and ESV were similar to those in the LV, although the differences were not statistically significant. While LGE and ECV remodeling were the major factors for identifying suspected myocarditis, global cardiac function measures (volumes, mass) did not show significant differences between suspected and excluded myocarditis cases within each referral group (groups 1 and 2). Furthermore, LVEF showed only significant difference between suspected and excluded myocarditis in group 1; but not in group 2. However, myocardial strain (in all directions) and strain rate (in the circumferential and radial directions) significantly differentiated between suspected and excluded myocarditis inside groups 1 and 2, respectively. All strain and strain rate parameters were significantly lower in the suspected myocarditis group than those in excluded myocarditis group (Table 1, Figure 1, Figure 2). On the regional level (base, mid-ventricle, apex), all strain measurements, except for the mid-ventricular and apical longitudinal strains, showed significant differences between suspected and excluded myocarditis. Furthermore, all strain rates, except for the mid-ventricular and apical longitudinal strain rates, showed significant differences between suspected and excluded myocarditis. There existed significant moderate-to-high correlations between the strain vs strain rate parameters (Figure 3). Furthermore, the strain and strain rate parameters had significant moderate-to-high positive correlations with LVEF and significant negative correlations with LV EDV, LV ESV, and LV mass. There existed also significant mild-to-moderate correlations between strain rates and RVEF.Discussion and Conclusions
The study results demonstrate the high sensitivity of strain and strain rate for differentiating between suspected and excluded myocarditis, which could be explained by the nature of these parameters for detecting subclinical cardiac dysfunction that may be present despite normal global cardiac function5. The results showed significant correlations between strain and strain rate parameters, which demonstrates that COVID-19 results in simultaneous deterioration of both systolic (strains) and diastolic (strain rates) cardiac functions. There were also associations between strain/strain rate versus global cardiac function parameters, which demonstrates that contractility deterioration occurs during an ongoing process of ventricular remodeling. This study also sheds the light on the limitations of conventional serum cardiac biomarkers, where several subjects with elevated biomarkers had myocarditis excluded by MRI, which emphasizes the limited specificity of these biomarkers. In conclusion, this study emphasizes the value strain and strain rate as sensitive parameters that can detect subclinical cardiac dysfunction in high-risk patients with suspected myocarditis in long COVID.Acknowledgements
Study supported by funding from Medical College of Wisconsin Clinical and Translational Science Institute (CTSI).References
1. Writing committee, T.J. Gluckman et al. J Am Coll Cardiol. 2022; 79:1717-1756.
2. V. Puntmann et al. JAMA Cardiol. 2020; 5:1265-1273.
3. B. Buckley et al. Eur J Clin Invest. 2021; 51: e13679.
4. V. Ferreira et al. J Am Coll Cardiol. 2018; 72: 3158-3179.
5. E. Ibrahim. Heart Mechanics. Magnetic Resonance Imaging. CRC Press. 2017.
Figures
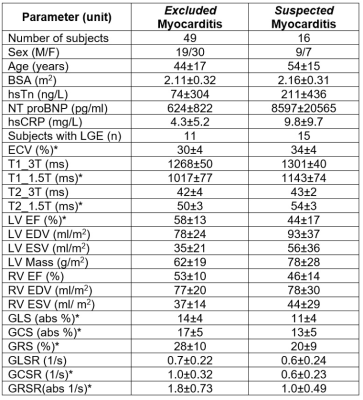
Table 1. Cardiac measurements (mean±SD) in excluded and
suspected myocarditis groups. Abbreviations: hsTn, cardiac troponin; NT proBNP, brain
natriuretic peptide; hsCRP, c-reactive protein; LGE, late gadolinium
enhancement; ECV, extracellular volume; EDV, end-diastolic volume; ESV,
end-systolic volume; GLS, GCS & GRS: global longitudinal, circumferential
& radial systolic strains; GLSR, GCSR & GRSR: global longitudinal,
circumferential & radial diastolic strain rates. ‘*’: statistical significance
(p<0.05).

Figure 1. (A) Longitudinal,
(B) circumferential, and (C) radial peak systolic strains shown for excluded
myocarditis vs suspected myocarditis groups at the global, basal,
mid-ventricular, and apical levels. Strains are always smaller in suspected
than in excluded myocarditis, where most differences are statistically
significant (*: P<0.05). Units are in absolute % for longitudinal and circumferential
strains (original values are negative).

Figure 2. (A) Longitudinal,
(B) circumferential, and (C) radial peak diastolic strain rates shown for
excluded myocarditis vs suspected myocarditis groups at the global, basal,
mid-ventricular, and apical levels. Strain rates are always smaller in
suspected than in excluded myocarditis, where most differences are
statistically significant (*: P<0.05). Units are in absolute 1/s for radial
strain rates (original values are negative).

Figure 3. Linear
regression and correlation coefficients for peak systolic strain vs peak
diastolic strain rate in the (A) longitudinal (GLS x GLSR), (B) circumferential
(GCS x GCSR), and radial (GRS x GRSR) directions. Significant high correlations
between strains and strain rates in all directions represent associated
deterioration in both systolic contraction and diastolic relaxation in
suspected vs excluded myocarditis.
DOI: https://doi.org/10.58530/2023/1904