1902
Structural Brain Differences and Cognitive Performance between patients with Long-COVID and Normal Recovery1University of British Columbia, Vancouver, BC, Canada, 2BC Children's Hospital Research Institute, Vancouver, BC, Canada, 3Vancouver Coastal Health, Vancouver, BC, Canada
Synopsis
Keywords: White Matter, COVID-19
Previous research suggests that COVID-19 infection may be associated with brain changes that are similar to a decade of aging.1 It is unknown whether symptom duration influences brain structure. We compared participants with COVID-19 symptoms for more than 2 months (long-COVID) (n=43) to participants who recovered within 2 months (normal recovery) (n=56). We assessed white matter with diffusion tensor imaging, regional brain volumes using Freesurfer, and cognition using the NIH Toolbox. Although the effect of age on MRI indices and cognition was readily detectable, we found no differences between long-COVID and normal recovery on brain structure or cognitive performance.Introduction
Common symptoms of long-COVID include memory problems and brain fog, however, their pathophysiology is unclear.2 This study aimed to determine if long-COVID is associated with i) differences in markers of white matter diffusivity in the brain, ii) differences in subcortical brain volumes in select regions of interest, and iii) lower scores on objective cognitive testing.Methods
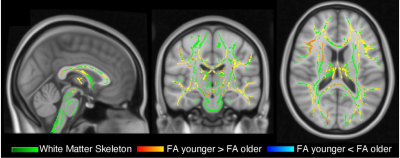
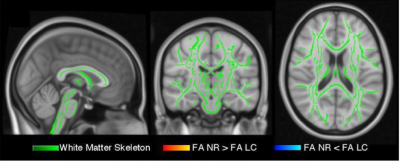
We compared individuals who experienced COVID-19 symptoms for more than 60 days post-infection (long-COVID) (n=43) to individuals who recovered from COVID-19 within 60 days of infection (normal recovery) (n=56). We collected information regarding physical and mental health, and COVID-19 illness. We administered the NIH Toolbox’s Cognition Domain. Participants underwent Magnetic Resonance Imaging (MRI) with Diffusion Tensor Imaging (DTI). We evaluated the effect of age on DTI metrics, regional brain volumes, and cognitive performance. Scans were obtained a mean of 5.5 months after a positive SARS-CoV-2 assay. Tract-based spatial statistics was used to perform a whole-brain voxel wise analysis on standard DTI metrics (FA, AD, MD, RD), controlling for age. Bilateral subregional cortical and subcortical volumes for regional brain volumes were extracted with FreeSurfer (7.2.0). Pial and white matter surface were manually edited to maximize segmentation accuracy. Volumetric comparisons included the hippocampus, amygdala, olfactory sulcus, Heschl’s gyrus, and parahippocampus as regions of interest (ROIs). We fit linear models with the ROI volume as the dependent variable and long-COVID vs normal recovery, age, sex, and intracranial volume as the independent variables. We used NIH Toolbox Fully Adjusted Scores, which adjust for age, sex, ethnicity, and level of education, to compare long-COVID and normal recovery groups with two-sample t-tests.Results
The long-COVID group had a mean age of 44.5 (18.1) years and 33 (59%) were female. The normal recovery group had a mean age of 46.2 (14.2) and 31 (74%) were female. Age Analysis: In a simple linear regression, age had a significant negative correlation with FA (p<0.001, β=-0.47 95% CI [-0.7, -0.2]). When grouping by decade, 10 years of older age was associated with worsened whole-brain white matter integrity and smaller subcortical brain volumes. Older age was associated with lower Fluid but not Crystallized cognitive scores (p<0.001 and p=0.52). COVID groups: DTI metrics, subcortical brain volumes, and Fluid and Crystallized Composite scores did not differ significantly between those with long-COVID vs those with normal recovery (all p>0.05). In exploratory analyses, the long-COVID group performed better than the normal recovery group on the List Sorting Working Memory subtest (puncorrected=0.04), however this was a relatively small effect (d=-0.43, 95% CI [-0.85, -0.01]) and did not survive correction for multiple comparison.Conclusions
We detected expected differences in brain structure and cognitive function associated with age. Although long-COVID patients reported neuropsychiatric symptoms, we did not find significant differences in cognitive performance or brain structure when compared to normal COVID patients.Acknowledgements
No acknowledgement found.References
1. Douaud, G., Lee, S., Alfaro-Almagro, F., Arthofer, C., Wang, C., McCarthy, P., Lange, F., Andersson, J. L. R., Griffanti, L., Duff, E., Jbabdi, S., Taschler, B., Keating, P., Winkler, A. M., Collins, R., Matthews, P. M., Allen, N., Miller, K. L., Nichols, T. E., & Smith, S. M. (2022, March 7). SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature, 604(7907), 697–707. https://doi.org/10.1038/s41586-022-04569-5
2. Méndez, R., Balanzá‐Martínez, V., Luperdi, S., Estrada, I., Latorre, A., González‐Jiménez, P., Feced, L., Bouzas, L., Yépez, K., Ferrando, A., Hervás, D., Zaldívar, E., Reyes, S., Berk,M., & Menéndez, R. (2021). Short‐term neuropsychiatric outcomes and quality of life in COVID‐19 survivors. Journal of Internal Medicine, 290(3), 621–631. https://doi.org/10.1111/joim.13262
Figures