1874
Comparison of calculated DWI and single-shot EPI DWI for prostate cancer detection at 3T1Radiology, Kawasaki Medical School, Kurashiki-city, Japan, 2Philips Japan, Tokyo, Japan, 3Radiology, Radiolonet Tokai, Nagoya, Japan
Synopsis
Keywords: Prostate, Prostate
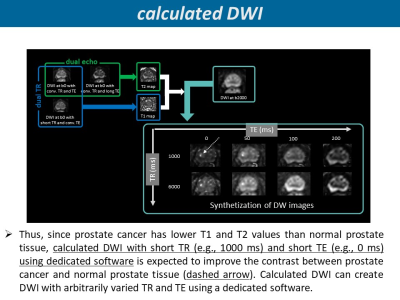
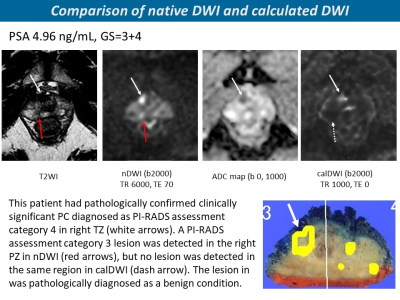
We compared diagnostic performance of clinically significant PC (csPC) between calculated DWI (calDWI) which enable to synthesize DW images with any TR and TE and native acquired single-shot EPI DWI (nDWI). The calDWI was generated with TR of 1000 and TE of 0 ms. Three radiologists independently assessed eight regions of each prostate by PI-RADS v 2.1 DWI score. For diagnostic performance of csPC, AUC was comparable between calDWI and nDWI in two readers. The diagnostic specificity was significantly higher in calDWI than in nDWI in two readers. Compared with nDWI, calDWI had similar or higher diagnostic performance in csPC.INTRODUCTION
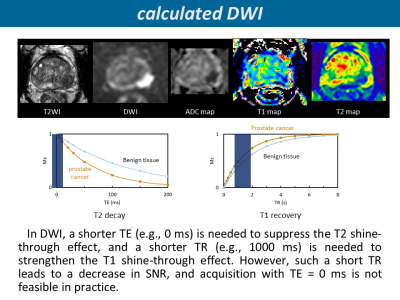
DWI is key component of multiparametric MRI (mpMRI) in prostate. However, single-shot echo-planar DWI (ssEPI DWI) with higher b-value more than 1400 s/mm2, which is commonly used in daily clinical practice, still shows insufficient image contrast between benign and malignant prostatic tissues. Recently, it has been reported that shorter TR can improve diffusion contrast compared to conventional (long) TR1, utilizing the prostate uniqueness that T1 of prostate cancer (PC) is lower than that of benign prostatic tissue2-4. However, such a short TR leads to a decrease in SNR. We have previously reported calculated DWI (calDWI) which enable to adjust any TR as well as any TE in prostate5. Compared to conventional native acquired ssEPI DWI (nDWI), calDWI with shorter TR and TE tended to have better diffusion contrast5. The purpose of this study is to compare diagnostic performance of clinically significant PC (csPC) between calDWI and nDWI.METHODS
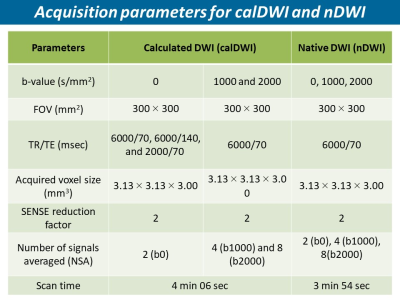
The subjects were 34 patients with csPC who underwent mpMRI on Ingenia Elition 3.0T (Philips Healthcare, Best, The Netherlands) and radical prostatectomy. For DWI with b-value of 2000 s/mm2 (b2000), nDWI was scanned with TR of 6000 and TE of 70 ms. CalDWI was generated with TR of 1000 ms to utilize T1 shine-through and TE of 0 ms to remove T2 shine-through completely. T2 shine-through in DW images is not efficient in prostate due to shorter T26 in PC. Three radiologists with 1 year (Reader 1), 11 years (Reader 2), and 25 years (Reader 3) of experience in prostate MRI interpretation) independently assessed eight prostate regions (six peripheral zone: right apex, right middle, right base, left apex, left middle, and left base; and two transition zones: right transition zone and left transition zone) of each patient by DWI score in PI-RADS v 2.17. PI-RADS v2.1 DWI score ≥3 was considered positive for csPC detection. First, only nDWI was evaluated first, and three weeks later, both nDWI and calDWI were evaluated in combination. In both sessions, T2-weighted imaging was used to provide anatomical information in addition to DW images. As another session, for the index lesion with the highest GS and largest size among the csPCs of each patient, qualitative lesion conspicuity score (LCS) based on 4-point Likert scales (1=invisible for surrounding normal site; 2=slightly high, 3=moderately high; 4=very high) and quantitative tumor contrast ratio (CR = (lesion mean signal intensity (LSI) - benign PZ mean signal intensity (BSI)) / (LSI+BSI)) were assessed.RESULTS
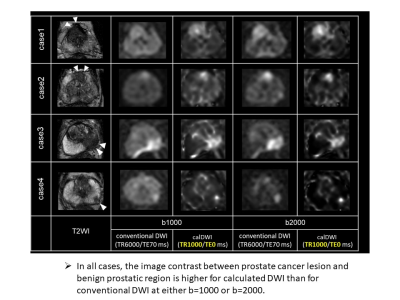
For diagnostic performance of csPC using DWI score, AUC was significantly higher in calDWI than in nDWI in reader 3 (0.855 vs. 0.805 in reader 3 (P=0.004)), and was comparable between calDWI and nDWI in reader 1 and 2 (0.731 vs. 0.716 in reader 2 (P=0.630) and 0.771 vs. 0.776 in reader 2 (P=0.728)). The diagnostic specificity was significantly higher in calDWI than in nDWI in reader 1 (0.758 vs. 0.608, P = 0.003) and reader 3 (0.900 vs. 0.683, P < 0.001, respectively), but not in reader 2 (0.717 vs. 0.775, P = 0.118). There was no significant difference in diagnostic sensitivity between nDWI and calDWI in three readers (0.700 to 0.767 vs. 0.658 to 0.775, P=0.052 to P=1.000). LCS was comparable between calDWI and nDWI in three readers (P=0.145 to P=0.967). CR in calDWI was significantly higher than that in nDWI (0.65±0.14 vs. 0.37±0.11, P < 0.001).DISCUSSION
Using prostatectomy as the reference standard, we compared diagnostic performance for csPC detection between nDWI and calDWI. The quantitative lesion conspicuities for csPC are higher in calDWI than in nDWI. This may be due to the increased signal intensity of PC lesion caused by the enhanced T1 shine-through effect from short TR and the decreased signal intensity of benign prostatic regions caused by the suppression of the T2 shine-through effect from the short TE. Regarding the diagnostic performance of csPC detection using the DWI score of PI-RADS v2.1 in PC patients who underwent prostatectomy, diagnostic sensitivity and AUC were comparable between nDWI and calDWI in three readers and two readers, respectively. However, the diagnostic specificity was higher in calDWI than tha in nDWI in two readers. This increase in diagnostic specificity for csPC, i.e., high true nagative and low false positive rates, should be attributed to the signal suppression of high-signal benign prostatic lesions such as chronic prostatitis and beign prostatic hyperplasia and high-signal benign prostatic structures including central zone and anterior fibromuscular stroma in DWI. The high contrast resolution between benign prostatic tissues and csPC and the high diagnostic specificity can be clinically beneficial for two situations. First, it will contribute to improving the diagnostic performance of radiologists and urologists who do not have sufficient experience in prostate MRI diagnosis. Second, the number of unnecessary biopsies and needle biopsies can be reduced.DISCUSSION
Compared with nDWI, calDWI had similar or higher diagnostic performance of csPC. In particular, high detection specificity for csPC in calDWI might be beneficial to avoid unnecessary biopsies.Acknowledgements
No acknowledgement found.References
1. Ueda Y, Tamada T, Yoshida K, et al. Short TR DWI in prostate. Proceedings of the 28th Annual Meeting of ISMRM, 2020 #2423.
2. Shiradkar R, Panda A, Leo P, et al. T1 and T2 MR fingerprinting measurements of prostate cancer and prostatitis correlate with deep learning-derived estimates of epithelium, lumen, and stromal composition on corresponding whole mount histopathology. Eur Radiol 2021; 31: 1336-46.
3. Baur ADJ, Hansen CM, Rogasch J, et al. Evaluation of T1 relaxation time in prostate cancer and benign prostate tissue using a Modified Look-Locker inversion recovery sequence. Sci Rep 2020;10(1):3121.
4. Panda A, Obmann VC , Lo WC, et al. MR fingerprinting and ADC mapping for characterization of lesions in the transition zone of the prostate gland. Radiology 2019; 292: 685-94.
5. Ueda Y, Tamada T, Sanai H, et al. Feasibility of synthetic short TR and short TE DWI in prostate cance. Proceedings of the 29th Annual Meeting of ISMRM, 2021 #3711
6. Liu W, Turkbey B, Sénégas J, et al. Accelerated T2 mapping for characterization of prostate cancer. Magn Reson Med 2011;65(5):1400-1406.
7. Turkbey B, Rosenkrantz AB, Haider MA, et al. Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol 2019;76(3):340-351.
Figures