1872
Reverse Encoding Distortion Correction for DWI: Improving Image Quality and Differention Capability of Malignant from Benign Prostatic Areas1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Joint Research Laboratory of Advanced Medical Imaging, Fujita Health University School of Medicine, Toyoake, Japan, 3Canon Medical Systems Corporation, Otawara, Japan, 4Fujita Health University Hospital, Toyoake, Japan
Synopsis
Keywords: Prostate, Cancer
We hypothesize that RDC is useful for image quality and diagnostic performance improvements on DWI with b value at 1500 s/mm2 in suspected prostatic cancer patients, although there was little influence of RDC on DWI at in vitro study. The purpose of this study was to determine the influence of RDC for ADC measurement at in vitro study and its’ utility for improving image quality and diagnostic performance of malignant from benign prostatic areas on prostatic DWI as in vivo study.Introduction
Diffusion-weighted imaging (DWI) is one of the key sequences for multiparametric MRI in suspected prostatic cancer and has been generally obtained by means of single-shot echo-planar imaging (EPI) as the current standard sequence (1-4). However, a major disadvantage of single-shot EPI is that it is considerably prone to artifacts, particularly susceptibility artifacts at tissue interfaces and image blurring, which even tend to increase at higher field strengths. Therefore, several approaches for DWI such as parallel transmit EPI or readout-segmented multi-shot EPI, reduced field-of-view (FOV) in the phase-encoding direction, and 2D navigator phase correction, etc. have been tested for improving image quality and reducing artifacts due to various causes (5-9). Under the above-mentioned situations, Canon Medical Systems Corporation introduces and clinically sets reverse encoding distortion correction (RDC) for body DWI with applying deep learning reconstruction (DLR) in 2022. However, no major reports are not assessed the capability of RDC for improving image quality and influence to ADC measurement accuracy on prostatic DWI. We hypothesize that RDC is useful for image quality and diagnostic performance improvements on DWI with b value at 1500 s/mm2 in suspected prostatic cancer patients. The purpose of this study was to determine the influence of RDC for ADC measurement at in vitro study and its’ utility for improving image quality and diagnostic performance of malignant from benign prostatic areas on prostatic DWI as in vivo study.Materials and Methods
For in vitro study, the quantitative diffusion phantom (High Precision Devices, Inc, Boulder, CO) developed by NIST/ QIBA consists of 13 vials filled with varying concentrations of polyvinylpyrrolidone in aqueous solution was scanned by DWIs with and without RDC to evaluate ADC measurement accuracy in this study. In addition, 40 suspected prostatic cancer patients underwent DWI at b value as 1500 s/mm2 with and without RDC at a 3T MR system and pathological examinations as in vivo study. According to the pathological examination results, 86 areas were determined as malignant areas, and 86 out of 394 areas were computationally selected as benign areas. On in vitro study, ADCs at each phantom on DWI with and without RDC were determined and correlated with standard reference by Pearson’s correlation analysis. In addition, ADC difference between DWIs with and without RDC at each phantom was compared by paired t-test. On in vivo study, signal to noise ratio (SNR) between benign prostatic area and muscle, contrast-noise ratio (CNR) between malignant and benign areas and ADCs in malignant and benign areas were determined by ROI measurements on each DWI. Moreover, overall image quality, artifact and lesion conspicuity were assessed by 5-point visual scoring system on each DWI. Then, paired t-test or Wilcoxon’s signed rank test were performed to compare SNR and qualitative indexes between DWIs with and without RDC technique (i.e. RDC DWI vs. DWI). To evaluate the affection of RDC for ADC measurements, ADCs from RDC DWIs were correlated with those from DWIs by Pearson’s correlation was performed. Moreover, ADC of each DWI were also compared between malignant and benign areas by Student’s t-test. Then, diagnostic performance of ADC was compared between RDC DWI and DWI by ROC analysis. Finally, sensitivity (SE), specificity (SP) and accuracy (AC) were compared between both ADCs by McNemar’s test.Results
Representative cases are shown in Figures 1. On in vitro study, Pearson’s correlation of ADC between each DWI and standard reference was determined as significant and excellent (RDC DWI: r=1.0, p<0.0001; DWI: r=0.999, p<0.0001). There were no significant differences of ADC between RDC DWI and DWI at each phantom (p>0.05). On in vivo study, compared results of quantitative and qualitative indexes are shown in Figure 2 and 3. SNR of RDC DWI was significantly higher than that of DWI (p<0.05). Overall image quality and artifact of RDC DWI were significantly better than those of DWI (p<0.05). On correlation of ADC between both DWIs, there were significant and good correction between RDC DWI and DWI (r=0.95, p<0.0001). When compared ADCs from RDC DWI and DWI in malignant and benign prostatic areas, ADC of malignant area was significantly lower than that of benign area (p<0.05). Compared diagnostic performance of ADC between RDC DWI and DWI are shown in Figure 4. Area under the curve (AUC), SP and AC of RDC DWI (AUC: 0.85, SP: 72.1%, AC: 79.1%) were significantly better than those of DWI without RDC (AUC: 0.79, p=0.008; SP: 64%, p=0.02; AC: 74.4%, p=0.008).Conclusion
Reverse encoding distortion correction (RDC) can improve the image quality of diffusion weighted images of the prostate and has the potential to improve lesion characterization in patients with suspected prostate cancer.Acknowledgements
This study was technically and financially supported by Canon Medical Systems Corporation.References
- Kayat Bittencourt L, Litjens G, et al. Prostate Cancer: The European Society of Urogenital Radiology Prostate Imaging Reporting and Data System Criteria for Predicting Extraprostatic Extension by Using 3-T Multiparametric MR Imaging. Radiology. 2015; 276(2): 479-489.
- Padhani AR, Barentsz J, Villeirs G, et al. PI-RADS Steering Committee: The PI-RADS Multiparametric MRI and MRI-directed Biopsy Pathway. Radiology. 2019; 292(2): 464-474.
- Barentsz JO, Richenberg J, Clements R, et al; European Society of Urogenital Radiology. ESUR prostate MR guidelines 2012. Eur Radiol. 2012; 22(4): 746-757.
- Turkbey B, Rosenkrantz AB, Haider MA, et al. Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol. 2019; 76(3): 340-351.
- Porter DA, Heidemann RM. High resolution diffusion-weighted imaging using readout-segmented echo-planar imaging, parallel imaging and a two-dimensional navigator-based reacquisition. Magn Reson Med. 2009; 62(2): 468-475.
- Setsompop K, Cohen-Adad J, Gagoski BA, et al. Improving diffusion MRI using simultaneous multi-slice echo planar imaging. Neuroimage. 2012; 63(1): 569-580.
- Yıldırım İO, Sağlık S, Çelik H. Conventional and ZOOMit DWI for Evaluation of Testis in Patients With Ipsilateral Varicocele. AJR Am J Roentgenol. 2017; 208(5): 1045-1050.
- Wilm BJ, Svensson J, Henning A, Pruessmann KP, Boesiger P, Kollias SS. Reduced field-of-view MRI using outer volume suppression for spinal cord diffusion imaging. Magn Reson Med. 2007; 57(3): 625-630.
- Gallichan D, Andersson JL, Jenkinson M, Robson MD, Miller KL. Reducing
distortions in diffusion-weighted echo planar imaging with a dual-echo
blip-reversed sequence. Magn Reson Med. 2010; 64(2): 382-390.
Figures
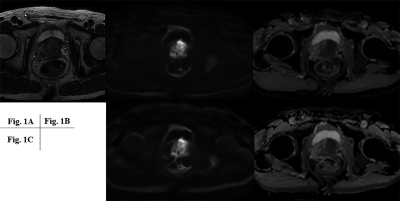
Figure 1. 78-year-old patient with prostatic cancer.
A: T2WI shows low signal intensity area from transitional zone to peripheral zone at basal level. B: (L to R: RDC DWI to ADC map from RDC DWI) Prostatic cancer is demonstrated as high signal intensity on RDC DWI and low ADC value on ADC map from transitional zone to peripheral zone at basal level. C: (L to R: RDC DWI to ADC map from DWI) Prostatic cancer is demonstrated as high signal intensity on DWI and low ADC value on ADC map from transitional zone to peripheral zone at basal level.
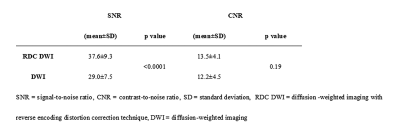
Figure 2. Compared results of quantitative index.
SNR had significant difference betweeb RDC DWI and DWI (p<0.05).
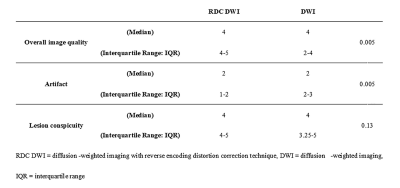
Figure 3. Compared results of qualitative indexes.
Overall image quality and artifact of RDC DWI were significantly higher or lower than those of DWI (p<0.05).
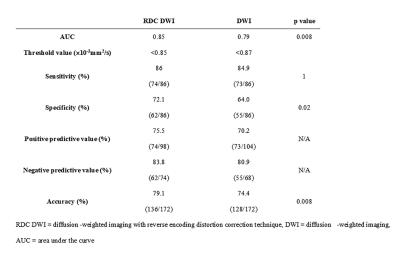
Figure 4. Compared diagnostic performance of ADC between RDC DWI and DWI.
Area under the curve (AUC), SP and AC of RDC DWI were significantly better than those of DWI (p<0.05).