1870
Sub-differentiation of intermediate risk prostate cancer by advanced diffusion-weighted imaging
Kun-Peng Zhou1, Hua-Bin Huang1, Long Liu1, Jie Bian2, and Li-Zhi Xie3
1Radiology, The Seventh Affiliated Hospital, Sun Yat-sen University, Shenzhen, China, 2Radiology, The second hospital of Dalian medical university, Dlian, China, 3GE Healthcare, Beijing, Beijing, China
1Radiology, The Seventh Affiliated Hospital, Sun Yat-sen University, Shenzhen, China, 2Radiology, The second hospital of Dalian medical university, Dlian, China, 3GE Healthcare, Beijing, Beijing, China
Synopsis
Keywords: Prostate, Prostate
The aim of this study was to investigate the use of advanced diffusion-weighted imaging to sub-differentiation of intermediate risk group PCa and aid treatment decision process. Finally, the logistic model was statistically significant, χ2=90.969, p<0.001. The model could correctly classify 86.40% of the subjects. The results of ROC analysis showed that area AUC was 0.9429, CI 95%: 0.9054-0.9805. Sensitivity, specificity, positive predictive value and negative predictive value were 88.06%, 84.31%, 88.06% and 84.31%, respectively. The results of this research may indicate that advanced diffusion-weighted imaging can sub-differentiate intermediate risk group PCa and aid the decision process of treatment.Introduction
Prostate cancer (PCa) is the most common non-cutaneous cancer in man, the incidence rate of PCa increased with age, about 85% of PCa patients are older than 65, and less than 1% are younger than 50(1). In order to select the appropriate treatment options and predict the prognosis of PCa patients, the NCCN Guidelines of PCa have incorporated a risk stratification scheme that uses a minimum of stage, Gleason grade, and prostate specific antigen (PSA) to assign patients to risk groups, including very low-, low-, favorable intermediate-, unfavorable intermediate-, high- and very high-risk group(2). For intermediate risk group PCa, some studies have showed that unfavorable intermediate-risk group (unFIRG)PCa patients had worse PSA recurrence-free survival and higher rates of distant metastasis and PCa-specific mortality than the favorable intermediate-risk group (FIRG) PCa patients(3). In recent years, some studies have demonstrated that diffusion weighted imaging (DWI) or advanced DWI could differentiate Gleason pattern ≤ 3 + 4 PCa and Gleason pattern ≥ 3 + 4 PCa. To our knowledge, the role of advanced DWI in the sub-differentiation of intermediate risk group PCa has not been reported. Therefore, the purpose of this study is sub-differentiation of intermediate risk group PCa using intravoxel incoherent motion (IVIM), stretched exponential model, and diffusion kurtosis imaging (DKI) to aid the treatment decision process.Methods
Our study was approved by the institutional review board and all patients signed informed consent at screening. 372 patients underwent prostate MRI examination at 3.0 T MRI (GE Discovery MR 750W) with 8-channel phased array coil, including conventional scanning sequences, IVIM, stretched exponential model and DKI. Finally, 118 intermediate-risk group PCa patients were included in the present study, including 51 FIRG PCa patients and 67 unFIRG PCa patients. Acquisition of quantitative data was carried on GE AW 4.6 workstation. ROI was then drawn on the parameter maps of IVIM, stretched exponential model and DKI. Three ROIs with area of 50 mm2 were randomly drawn at the maximum slicer of the lesion, and the average value was recorded. In order to examine the association between parameters of DKI, IVIM, and stretched exponential model with the probability of unFIRG PCa in intermediate risk group PCa, binary logistic regression analysis was applied. After binary logistic regression analysis, the receiver operating characteristic (ROC) curve of combination parameters, which were statistically significant in binary logistic regression analysis, were analyzed to test the diagnostic efficiency of detecting unFIRG PCa in intermediate risk group PCa.Results
A total of 118 intermediate-risk group PCa patients were included, including 51 patients were FIRG (Figure 1), and 67 patients were unFIRG (Figure 2). Finally, the logistic model was statistically significant, χ2=90.969, p<0.001. The model could correctly classify 86.40% of the subjects. FA (p<0.001), MD (p=0.031), MK (p=0.014), D (p=0.041), DDC (p=0.001) were statistically significant. Odds ratio (CI 95%) were 6.856 (2.679-17.545), 3.597 (1.292-10.013), 3.018 (1.107-8.227), 0.411 (0.175-0.962), 0.177 (0.062-0.510), respectively (Figure 3). The results of ROC analysis showed that area under the curve (AUC) was 0.9429, CI 95%: 0.9054-0.9805. Sensitivity, specificity, positive predictive value and negative predictive value were 88.06%, 84.31%, 88.06% and 84.31%, respectively.Discussion
This study used advanced DWI (IVIM, stretched exponential model and DKI) to differentiate FIRG group PCa and unFIRG PCa in intermediate risk group PCa. The results showed that combination of parameter D of IVIM, parameter DDC of stretched exponential model and parameters FA, MD and MK of DKI have ability to differentiate FIRG group PCa and unFIRG PCa in intermediate risk group PCa and have high diagnostic efficacy for unFIRG group PCa. This may be attributed to the difference in histological changes of FIRG group PCa and unFIRG group PCa, including vascular (i.e., capillaries), fibromuscular stroma, epithelium, and glandular lumen. Compared with FIRG group PCa, unFIRG group PCa contains increased volumes of low- restriction diffusivity epithelial cells and decreased high-restriction diffusivity stroma and lumen space. In this study, parameters pseudodiffusion coefficient (D*) and perfusion fraction (f) of IVIM, parameter heterogeneity index (α) of stretched exponential model also have no statistical significance. A reasonable explanation may be that the perfusion difference between FIRG group PCa and unFIRG group PCa may not be enough to be detected by D* and f in TZ.Acknowledgements
No acknowledgement found.References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30.
2. Schaeffer E, Srinivas S, Antonarakis ES, Armstrong AJ, Bekelman JE, Cheng H, et al. NCCN Guidelines Insights: Prostate Cancer, Version 1.2021. J Natl Compr Canc Netw. 2021;19(2):134-43.
3. Zumsteg ZS, Spratt DE, Pei I, Zhang Z, Yamada Y, Kollmeier M, et al. A new risk classification system for therapeutic decision making with intermediate-risk prostate cancer patients undergoing dose-escalated external-beam radiation therapy. Eur Urol. 2013;64(6):895-902.
Figures
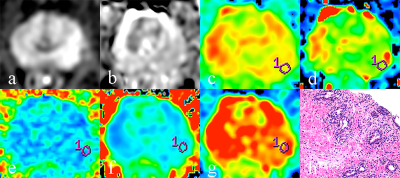
A 79-year-old FIRG group PCa patient and PSA of 13.45 ng/ml. (a, b) The lesion in the lift middle peripheral zone. (c) Diffusion coefficient (D) of 0.513×10-3mm2/s. (d) Distribute diffusion coefficient (DDC) of 0.494×10-3mm2/s. (e) Fractional anisotropy (FA) of 0.327. (f) Mean diffusion (MD) of 0.792×10-3mm2/s. (g) Mean kurtosis (MK) of 0.712. (h) HE staining, ×100.
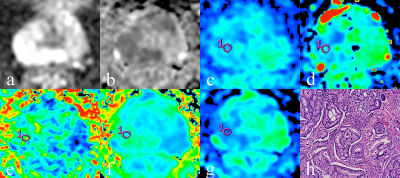
A 74-year-old unFIRG group PCa patient and PSA of 17.26 ng/ml. (a, b) The lesion in the right middle peripheral zone. (c) Diffusion coefficient (D) of 0.472×10-3mm2/s. (d) Distribute diffusion coefficient (DDC) of 0.458×10-3mm2/s. (e) Fractional anisotropy (FA) of 0.405. (f) Mean diffusion (MD) of 0.727×10-3mm2/s. (g) Mean kurtosis (MK) of 0.793. (h) HE staining, ×100.
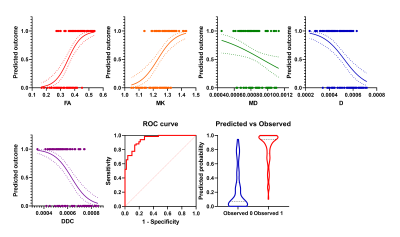
The results of binary logistic regression analysis showed that in intermediate risk group PCa, the prevalence of unFIRG PCa increased with the increase of FA value and MK value but decreased with the increase of MD value, D value, and DDC value. The diagnostic efficiency in distinguishing unFIRG PCa from intermediate risk group PCa of these parameters was 0.9429.
DOI: https://doi.org/10.58530/2023/1870