1797
New high-performance whole-body gradients to clarify Intravoxel incoherent motion DWI based multi-parametric MRI of prostate: Initial results1School of Engineering Medicine, Texas A&M University, Houston, TX, United States, 2Veterinary Clinical Sciences, University of Minnesota, Saint Paul, MN, United States, 3Center for Magnetic Resonance Research, University of Minnesota, Minneapolis, MN, United States, 4Siemens Healthcare, Erlangen, Germany
Synopsis
Keywords: Quantitative Imaging, Prostate, multi parametric MRI
We demonstrate the feasibility of obtaining high b-value (b > 2400 s/mm2) DWI images of the prostate obtained with short echo times (TE ~ 50 ms) on a prototype high-performance whole-body gradient system (Gmax = 200 mT/m, and SRmax = 200 T/m/s). Preliminary results from volunteers suggest that the apparent differences in the perfusion fraction metric of the IVIM model between the transition and peripheral zones of the prostate partly can be substantially diminished by choosing a shorter TE using high-performance gradients.Introduction
More than two-thirds (70-80%) of prostate cancers originate in the glandular-tissue-rich peripheral zone (PZ), and slightly less than a third from glandular-tissue-poor transition zone (TZ) of the prostate gland. Multi-parametric MRI (mpMRI) – a trio of T2-weighted (T2w), diffusion-weighed (DWI), and dynamic contrast-enhanced MRI (DCE-MRI) sequences - is the recommended initial diagnostic test for men with suspected prostate cancer1, with T2w and DWI imaging playing a primary role in the evaluation of lesions in the transition zone (TZ), peripheral zone (PZ) respectively. Although the sensitivity of mpMRI is high, the test lacks specificity. Two contributing factors include (a) the prolongation of echo time (TE) needed to obtain a high-b value EPI based DWI (b >= 1400 s/mm2, as recommended by PI-RADS v2.1)2 in prostate which is surrounded by air-tissue interfaces (rectum) using conventional gradients lowers the SNR as well as makes data acquisition susceptible to image distortion, and (b) while in principle, the intra-voxel incoherent motion model of diffusion (IVIM) can provide information on tissue diffusion and perfusion, the estimation of IVIM model parameters related to perfusion – perfusion fraction (f) and pseudo-diffusion (Df) – has remained a vexing problem3.In this work, we demonstrate the technical feasibility of obtaining high-b value, high-resolution DWI of the prostate gland using a whole-body, high performance gradient system with a peak gradient strength of 200 mT/m, and a peak slew rate of 200 T/m/s. Our results also show that the blood volume fraction (f) estimated from IVIM model is significantly affected by the choice of TE due to the significant difference in T2 between tissue and perfusion compartments.
Materials and Methods
Patient population: 5 male subjects (64.2 ± 9.1 yrs) provided written informed consent.MRI data acquisition: On a prototype Siemens Healthcare 3T system equipped with high-performance gradients (peak strength: 200 mT/m, peak SR: 200 T/m/s), the following data were acquired:
T2 weighted images: Prostate gland in at least two orthogonal orientations: TR/TE: 6010 ms/105 ms; voxel size: 0.6 x 0.6 x 3 mm3 (reconstructed as 0.3 x 0.3x 3 mm3); PAT acceleration factor = 4; scan time: 1:23 min; Deep learning reconstruction = on.
T2 map of prostate gland: TE1/ΔTE/TR/n_echoes = 10.5ms/10.5ms/2430ms/8; voxel size: 0.5 x 0.5 x 3 mm3; partial Fourier = 6/8; scan time: 10:16 min.
EPI-DWI ZOMit: FOV: 200 x 100 mm² (RFOV excitation); Acceleration factor: 2; TR/TE: 5000ms/100ms; Monopolar diffusion weighting; b-values: 0 (4 Av, 20, 50, 100 200, 200, 800, 1600 (6Av), 3200 (13 Av s/mm2; partial Fourier = 7/8; Deep-Resolve = on; BW/pixel: 1862 Hz/pixel; scan time: 8: 57min.The same protocol was repeated with echo-times of 80ms, 60ms, and 54ms.
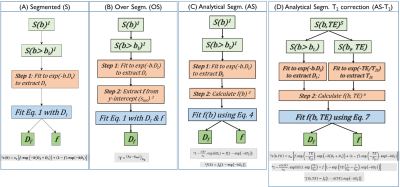
Data Analysis: IVIM model parameters from DWI at each TE were calculated using an analytical-segmented (AS) approach described previously4,5. The algorithmic steps are outlined in Figure 1.
Results
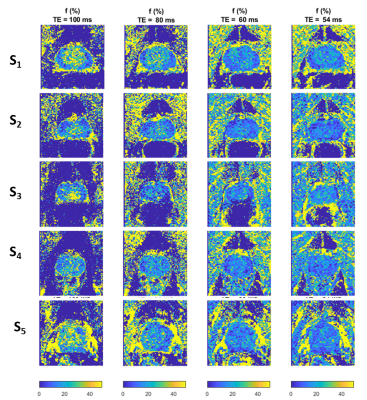
Calculated perfusion fraction map (f) as a function of TE for each of the five subjects is shown in Figure 2. The perfusion volume fraction in the transition zone of the prostate nearly doubles from 13.7% to 266.1% as TE increases from 54ms to 100ms. In contrast, f in the peripheral zone of the prostate is less affected. Note the apparent difference in f map between the PZ and TZ of the prostate gland which appears at longer TEs substantially less conspicuous at shorter TE.Conclusions
To our knowledge, these are the first results of high-b value (b = 3200 s/mm2) DWI of the prostate gland obtained with a whole-body, high performance gradient system with a peak gradient strength of 200 mT/m and a peak slew rate of 200 T/m/s. Our initial findings suggest that the what appears to be a large blood-volume fraction (f) difference between the PZ and TZ is instead likely due to the intrinsic T2 differences between the two compartments. These preliminary findings must be confirmed in a larger study.Acknowledgements
No acknowledgement found.References
1. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer—2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent | Elsevier Enhanced Reader. doi:10.1016/j.eururo.2020.09.042
2. PIRADS-V2-1.pdf. Accessed July 7, 2022. https://www.acr.org/-/media/ACR/Files/RADS/PI-RADS/PIRADS-V2-1.pdf
3. Shan Y, Chen X, Liu K, Zeng M, Zhou J. Prostate cancer aggressive prediction: preponderant diagnostic performances of intravoxel incoherent motion (IVIM) imaging and diffusion kurtosis imaging (DKI) beyond ADC at 3.0 T scanner with gleason score at final pathology. Abdom Radiol. 2019;44(10):3441-3452. doi:10.1007/s00261-019-02075-3
4. Buko E, Zhang J, Ajala A, Hor PH, Muthupillai R. An Analytical Segmented (AS) Approach for Extracting IntraVoxel Incoherent Motion (IVIM) Model Parameters.; 2018.
5. Buko E, Ajala A, Zhang J, Hor PH, Muthupillai R. An Analytical Segmented Approach for Extracting TE Independent Perfusion Fraction in Intravoxel Incoherent Motion (IVIM) MRI.; 2020.
Figures