1792
Validation of a new method for Quantifying CBF with IVIM
Mira Liu1, Chisondi Simba Warioba1, Julian Bertini1, Niloufar Saadat2, Timothy Carroll1, and Gregory Christoforidis2
1University of Chicago, Chicago, IL, United States, 2Interventional Radiology, University of Chicago, Chicago, IL, United States
1University of Chicago, Chicago, IL, United States, 2Interventional Radiology, University of Chicago, Chicago, IL, United States
Synopsis
Keywords: Quantitative Imaging, Perfusion
Intravoxel Incoherent Motion (IVIM) is a non-contrast MR diffusion-based scan that uses a multitude of b-values to measure various speeds of molecular perfusion and diffusion, sidestepping problems of Gd-contrast or increased transit time in neurovascular disease. Quantification of IVIM CBF in ml/100g/min using pseudo-diffusion mean transit time led to strong Wilcoxon signed rank agreement, similar sensitivity, and a small offset compared to microsphere perfusion across three physiologic states. This suggests IVIM can be used to quantify CBF in ml/100g/min in a setting of cerebral steno-occlusive disease.Introduction
Intravoxel Incoherent Motion (IVIM) is a non-contrast MR diffusion-based scan that uses a range of b-values to measure various speeds of molecular perfusion and diffusion, avoiding problems of Gd-contrast. Questions remain as to whether IVIM is quantitative and accurate in a setting of pathology. Quantification of cerebral blood flow (qCBF) proves a critical step in generalizability and consistent application at the clinical and research level as it will allow large longitudinal and multicenter trials and may avoid the confounding factors of relative CBF[2]. In this study we test an IVIM quantification factor that avoids assumptions regarding microvasculature and capillary beds and compare the resulting qCBF against gold-standard microspheres across three physiologic states (baseline, CO2 challenge and middle cerebral artery occlusion) in a pre-clinical canine model.Methods and Materials
Experimental methods: Five subjects underwent a two-day controlled experiment of a pre-clinical canine model of normocapnia, CO2 induced hypercapnia, and middle cerebral artery occlusion (ischemic stroke) with both IVIM and microsphere perfusion. For these five subjects, we required stable physiology (HR, BP, ETCO2 (elevated or nominal), body temp, etc.) throughout the experiments and perfusion was measured with quantitative neutron capture microsphere deposition and IVIM. Diffusion weighted images (2D single shot EPI, TR/TE= 3056/91ms, slices/thickness = 50/2mm, SENSE Factor=2) were collected with 10 b-values from 0 to 1000 s/mm2 (0,111, 222, 333, 444, 556, 667, 778, 889, 1000) and 3 orthogonal directions to ensure a clinically feasible scan time (5:38 min). Perfusion and diffusion values were calculated from the IVIM scan using software developed in-house with a two-step fit algorithm validated by simulations. Images of CBF at all states are produced with voxel-by-voxel fD* (Fig. 1a-c). Gold-standard neutron capture microsphere CBF was acquired with 4mL of stable isotope labeled 15μm microspheres injected in the left ventricle and blood withdrawn 10ml/min mid abdominal aorta analyzed through neutron activation at an independent laboratory (BioPal Inc. Medford, MA, USA). Hemispheric regions of interest were drawn on diffusion images to avoid bias, with cerebrospinal fluid voxels excluded (Fig. 1d).Pseudo-diffusion Mean Transit Time: Calibration of IVIM parameters to quantitative flow was calculated with the 3D probability distribution. MTT is the time it takes for half of the original molecules diffusing on average from the center of the voxel to have left the voxel. Knowing this, MTT can be calculated by solving the 3D diffusion probability distribution as a function of diffusivity for the time at which 50% of the molecules have traveled outside of the voxel from the center (Fig. 2). qCBF in ml/100g/min can then be calculated with this MTT using the central volume theorem[3]. Using this one can solve the 3D gaussian probability distribution as a function of time and diffusivity to determine IVIM qCBF in ml/100g/min.
Statistical Analysis: Hemispheric IVIM qCBF was compared to microsphere perfusion with linear regression to test sensitivity to physiologic state. Wilcoxon paired signed rank statistic and Bland-Altman analysis was calculated to study agreement and bias of IVIM qCBF compared to reference standard microspheres.
Results
IVIM qCBF showed response to changing physiologic state (Fig. 1) and linear regression returned linear agreement and correlation to microspheres across physiologic state (Fig. 3a). Wilcoxon paired signed rank statistic = 317 and p-value =.44 showed no statistically significant difference between IVIM qCBF and microsphere perfusion. Bland-Altman analysis (Fig. 3b) returned a small mean difference = 5.9, and 95% CI [-51.8, 63.6] centered about zero.Discussion
IVIM quantification using pseudo-diffusion mean transit time agreed with gold-standard microspheres across three physiologic states. Linear regression supported slightly lower sensitivity of IVIM qCBF to physiologic stress compared to microspheres. Wilcoxon signed-rank with a p-value of .44 showed quantification of IVIM returned no statistically significant difference from hemispheric microsphere perfusion (p>.10) on a paired-voxel-wise basis at baseline, post Co2-inhalation, and post-MCA occlusion. Bland-Altman analysis suggested minimal bias across all states. Limitations include varying physiology due to differences in timing, imperfect agreement of regions of interest compared to physical excision, and small pilot-study sample size. Cerebrospinal fluid in subarachnoid space and ventricles was avoided via manual segmentation and DWI thresholding. Though potential contamination may contribute to higher offset, IVIM qCBF quantified with MTT did return linear correlation, minimal bias, and strong Wilcoxon signed rank agreement compared to reference standard microspheres.Conclusion
Quantification of IVIM CBF in ml/100g/min using pseudo-diffusion mean transit time led to strong Wilcoxon signed rank agreement with microspheres, and linear correlation with minimal bias or offset across three physiologic states. This suggests it could be used to quantify CBF in ml/100g/min across different hemodynamic states and in a setting of cerebral steno-occlusive disease.Acknowledgements
Research reported in this publication is supported by NSF Fellowship NSF DGE-1746045, NIH Grant R01NS093908, and NIH Training Grant 5R25GM109439-09.References
1. Le Bihan, D., What can we see with IVIM MRI? Neuroimage, 2019. 187: p. 56-67.
2. Liu, M., et al., Augmentation of perfusion with simultaneous vasodilator and inotropic agents in experimental acute middle cerebral artery occlusion: a pilot study. J Neurointerv Surg, 2022.
3. Mihara, F., et al., Semi-quantitative CBF and CBF ratios obtained using perfusion-weighted MR imaging. Neuroreport, 2003. 14(5): p. 725-7.
Figures
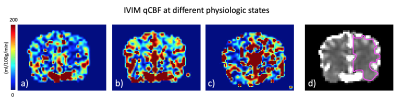
Figure 1. IVIM at a) baseline, 2) Co2-inhalation induced hypercapnia and c) post-MCA occlusion. Shown in d) is a cerebrospinal fluid mask on DWI and a hemispheric region of interest drawn manually avoiding ventricles and subarachnoid space.

Figure 2. On the left 1D shows the location along
the x-axis and the probability of its location along the y-axis. At time t with diffusion
coefficient D there is a 50% chance it has left the red range, shown with the equation in the center. On the right is a visual representation of this in 3D, with red showing the sphere beyond which a molecule has 50% chance of moving past.
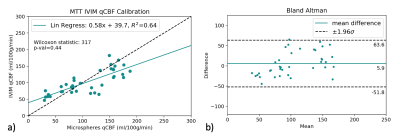
Figure 3. a) Linear regression between Microspheres and IVIM CBF quantified using a calibration coefficient calculated from pseudo-diffusion mean transit time and b) the corresponding Bland-Altman.
DOI: https://doi.org/10.58530/2023/1792