1746
Pretreatment Apparent Diffusion Coefficient Value for Prediction of Relapsed and Refractory Primary Central Nervous System Lymphoma1Chi Mei Medical Center, Tainan, Taiwan, 2Department of Health and Nutrition, Chia Nan University of Pharmacy and Science, Tainan, Taiwan, 3Department of Radiology, E-DA Hospital, I-Shou University, Kaohsiung, Taiwan, 4Department of Radiological Sciences, University of California, Irvine, CA, United States
Synopsis
Keywords: Tumors, Cancer
A subset of primary central nervous system lymphoma (PCNSL) may show early relapsed/refractory (R/R) disease after treatments. This study investigated the role of pretreatment apparent diffusion coefficient (ADC) values for the prediction of R/R in PCNSL. Total 52 patients with pathologically confirmed PCNSL were included, and 24 (46.2%) patients developed R/R (median time to relapse, 13 months) after treatment. The results showed female sex, complete response to first-line chemotherapy, and ADC value/ratio were significant predictors of R/R in PCNSL. Pretreatment ADC values/ratios offer objective and valuable evaluation for the treatment planning in PCNSL.Background and Purpose
Primary central nervous system lymphoma (PCNSL) accounts for 3-4% of central nervous system (CNS) tumors and 1-2% of non-Hodgkin’s lymphomas (NHLs) [1,2]. Diffuse large B- cell lymphoma (DLBCL) is the most common subtype of PCNSL [3]. There are no optimal standard treatments in PCNSL, and high-dose (HD) methotrexate (MTX)-based chemotherapy is the cornerstone of therapy in PCNSL. Although MTX-based chemotherapy and whole-brain radiotherapy (WBRT) have been considered to be effective therapies for PCNSL [4,5], up to 50-60% of patients eventually had relapsed/refractory (R/R) disease [6,7]. Although MRI findings such as tumor size, infratentorial localization, and hyperintense T2-fluid attenuated inversion recovery (FLAIR) lesion have been reported as important parameters associated with R/R in PCNSL [8], most reported imaging finding are qualitative and subjective. Thus, we investigated the role of pretreatment apparent diffusion coefficient (ADC) value on diffusion-weighted imaging (DWI) for the prediction of R/R in PCNSL.Materials and Methods
This retrospective study included patients with pretreatment brain MRI including DWI and corresponding ADC imaging and were sequentially diagnosed with PCNSL by pathological confirmation. All patients received HD-MTX based chemotherapy. Only patients with at least MRI follow-ups two times after treatments were included. From January 2006 to December 2021, total 52 patients (23 men and 29 women with median age 64 years) were included. The median follow-up time was 26.3 months. In 24 (24/52, 46.2%) patients with early R/R, the median time to R/R was 13 months. Preoperative brain MRI images were acquired using a 1.5-T (N = 48) (Siemens Avanto, Siemens Aera, or GE Signa) or a 3-T (GE Discovery MR750) (N = 4) MR scanner, equipped with eight-channel head coils in each machine. The protocols of MR imaging were as the following: axial and sagittal spin-echo T1WI, fast spin-echo T2WI, fluid attenuated inversion recovery (FLAIR). Contrast-enhanced images were obtained in axial and coronal T1WI. The DWI was performed by applying sequentially in the x, y, and z direction with b =1000 sec/mm2 or 1500 sec/mm2, and ADC maps were obtained from these imaging data. For ADC measurement, a circular ROI (area ranging from 20 to 64 mm2) was placed within the tumor area. For normalization of individual variance, ADC ratio was calculated by dividing the ADC value of the tumor by the ADC value of contralateral normal-appearing cerebral white matter (NAWM) in the same patient.Results
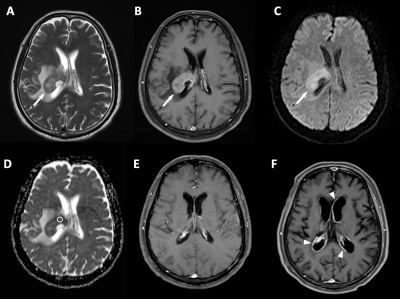
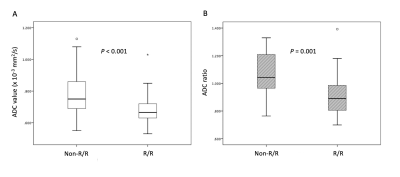
Of the 52 patients, 24 (24/52, 46.2%) PCNSL patients had developed R/R after treatments (Fig. 1), and 18 (18/52, 34.6%) patients died. Female sex and non-complete response (CR) after first-line chemotherapy were more frequent in the R/R group than in those without R/R (P < 0.05). The median ADC values and ADC ratios were lower in the R/R group than in those without R/R (P < 0.05) (Fig. 2). The cut-off points for the ADC value and ADC ratio were 0.68 x 10-3 mm2/sec and 0.97, respectively. An AUC of 0.78 and 0.77 were obtained for the ADC value and ADC ratio, respectively. When comparing the tumor progression survival (PSF), patients with lower ADC values and lower ADC ratios exhibited shorter PFS. On multivariate analysis, failure of CR to first-line chemotherapy and low ADC value were significant predictors of R/R (P < 0.05) with a hazard ratio of 5.22 and 14.45, respectively.Conclusions
The pretherapeutic quantitative ADC values and ratios offer valuable information for the treatment planning in PCNSL, such as the choice of chemotherapy agents, and decision on further consolidation therapy with stem cell transplantation or radiotherapy.Acknowledgements
No acknowledgement found.References
1. Hoffman, S.; Propp, J.M.; McCarthy, B.J. Temporal trends in incidence of primary brain tumors in the United States, 1985- 1999. Neuro-oncology 2006, 8, 27-37, doi:10.1215/s1522851705000323.
2. Villano, J.L.; Koshy, M.; Shaikh, H.; Dolecek, T.A.; McCarthy, B.J. Age, gender, and racial differences in incidence and survival in primary CNS lymphoma. British journal of cancer 2011, 105, 1414-1418, doi:10.1038/bjc.2011.357.
3. Montesinos-Rongen, M.; Brunn, A.; Bentink, S.; Basso, K.; Lim, W.K.; Klapper, W.; Schaller, C.; Reifenberger, G.; Rubenstein, J.; Wiestler, O.D.; et al. Gene expression profiling suggests primary central nervous system lymphomas to be derived from a late germinal center B cell. Leukemia 2008, 22, 400-405, doi:10.1038/sj.leu.2405019.
4. Morris, P.G.; Abrey, L.E. Therapeutic challenges in primary CNS lymphoma. Lancet Neurol 2009, 8, 581-592, doi:10.1016/s1474-4422(09)70091-2.
5. Song, J.; Samant, R.; Jay, M.; Chaudry, H.; Fan, X.Y.; MacDonald, D.; Bence-Bruckler, I.; Nair, V. Whole brain radiotherapy improves survival outcomes in primary CNS lymphoma patients ineligible for systemic therapy. Supportive Care in Cancer 2020, 28, 5363-5369, doi:10.1007/s00520-020-05376-2.
6. Grommes, C.; DeAngelis, L.M. Primary CNS Lymphoma. Journal of Clinical Oncology 2017, 35, 2410-2418, doi:10.1200/jco.2017.72.7602.
7. Korfel, A.; Schlegel, U.; Herrlinger, U.; Dreyling, M.; Schmidt, C.; von Baumgarten, L.; Pezzutto, A.; Grobosch, T.; Kebir, S.; Thiel, E.; et al. Phase II Trial of Temsirolimus for Relapsed/Refractory Primary CNS Lymphoma. J Clin Oncol 2016, 34, 1757- 1763, doi:10.1200/jco.2015.64.9897.
8. Tabouret, E.; Houillier, C.; Martin-Duverneuil, N.; Blonski, M.; Soussain, C.; Ghesquières, H.; Houot, R.; Larrieu, D.; Soubeyran, P.; Gressin, R.; et al. Patterns of response and relapse in primary CNS lymphomas after first-line chemotherapy: imaging analysis of the ANOCEF-GOELAMS prospective randomized trial. Neuro-oncology 2017, 19, 422-429, doi:10.1093/neuonc/now238.
Figures