1719
Interaction Between ACTH and Hippocampal Dynamic Functional Connectivity onPersonality Traits in Bipolar Disorder with Suicidal Attempt
Pan Chen1, Ying Wang1, Shuming Zhong2, Guanmao Chen1, and Long Qian3
1Medical Imaging Center, First Affiliated Hospital of Jinan University, Guangzhou, China, 2MR Research, GE Healthcare, Guangzhou, China, 3MR Research, GE Healthcare, Beijing, China
1Medical Imaging Center, First Affiliated Hospital of Jinan University, Guangzhou, China, 2MR Research, GE Healthcare, Guangzhou, China, 3MR Research, GE Healthcare, Beijing, China
Synopsis
Keywords: Neuroinflammation, Brain Connectivity
The goal of this study was to investigate the underlying mechanisms of suicidal behavior by detecting the dynamic functional connectivity (dFC) variability of hippocampus and HPA axis activity, as well as their relationship with personality traits in BD with suicidal attempt (SA). We assessed the activity of the HPA axis by measuring morning plasma adrenocorticotropic hormone (ACTH) and cortisol (CORT) levels. All participants underwent personality assessment using Minnesota Multiphasic Personality Inventory-2. BD with SA exhibited increased dFC variability of the hippocampal-temporal cortex and less HPA axis hyperactivity, which may both together lead to the possibility of changes in personality traits.Background
Suicide in bipolar disorder (BD) is a multi-determined behavior, involving specific neuroendocrine and psychological mechanisms. The goal of this current study was to investigate the underlying mechanisms of suicidal behavior by detecting the dynamic functional connectivity (dFC) variability of hippocampus and HPA axis activity, as well as their relationship with personality traits in BD with suicidal attempt (SA).Methods
Resting-state functional magnetic resonance imaging (fMRI) data were collected from a sample group of 79 patients with BD (39 with SA and 40 without SA), and 35 healthy controls (HCs). The severity of depressive symptoms was evaluated by 24-item HDRS, the severity of manic symptoms was evaluated by YMRS, and the severity of suicidal ideation was evaluated by SSI-Beck.MRI scanning was performed within 48 h of initial contact. All MRI data were obtained on a GE Discovery MR750 3.0T system with an 8-channel phased-array head coil. The participants were scanned in a supine, head-first position with symmetrically placed cushions on both sides of the head to decrease motion. During the scanning, the participants were instructed to relax with their eyes closed without falling asleep. After the experiment, each participant confirmed not having fallen asleep. The rs-fMRI data were acquired using a gradient-echo echo-planar imaging sequence with the following parameters: time repetition (TR)/time echo (TE) = 2000/25 ms; flip angle = 90°; voxel size = 3.75 × 3.75 × 3 mm3; field of view (FOV) = 240 × 240 mm2; matrix = 64 × 64; slice thickness/gap = 3.0/1.0 mm; 35 axial slices covering the whole brain; and 210 volumes acquired in 7 min.
seed-based dFC analyses were performed by placing bilateral regions of interest (ROIs) within 4 non-overlapping masks (the bilateral rostral hippocampus and the bilateral caudal hippocampus) using Brainnetome atlas.
We assessed the activity of the HPA axis by measuring morning plasma adrenocorticotropic hormone (ACTH) and cortisol (CORT) levels. All participants underwent personality assessment using Minnesota Multiphasic Personality Inventory-2 (MMPI-2).
Results
SA group exhibited lower ACTH and increased dFC variability between the right caudal hippocampus and the left superior temporal gyrus (STG) when compared to the non-SA group. Meanwhile, for BD with SA, ACTH was positively correlated with dFC variability between the right caudal hippocampus and the left STG. The SA group scored significantly higher on Hypochondriasis, Depression, and Schizophrenia than the non-SA group. Additionally, the interaction of ACTH × dFC variability between the right caudal hippocampus and left STG was an independent contributor for Depression score in the SA group.Conclusions
Our findings suggested that BD patients with SA exhibited increased dFC variability of the hippocampal-temporal cortex and less HPA axis hyperactivity, both significantly positively correlated. And BD with SA have more abnormal personality traits than non-suicidal BD patients. In addition, the interaction of ACTH × dFC variability between the right caudal hippocampus and left STG was an independent contributor for the Depression score of MMPI-2 in BD with SA, suggesting that abnormal HPA axis and dFC variability in hippocampal-STG may together lead to the possibility of changes in personality traits. Our results illustrate the importance of combining neuroendocrine and psychological changes to investigate the underlying mechanisms of suicidal behavior in BD.Acknowledgements
We gratefully acknowledge funding provided by the following National Natural Science Foundation of China, China (No: 81801347; 81971597), Guangdong Basic and Applied BasicResearch Foundation (No: 2021A1515011034; 2021A1515110130), Planned Science andTechnology Project of Guangdong Province, China (No: 2017B020227011), Project in BasicResearch and Applied Basic Research in General Colleges and Universities of Guangdong, China(No: 2018KZDXM009)References
No reference found.Figures
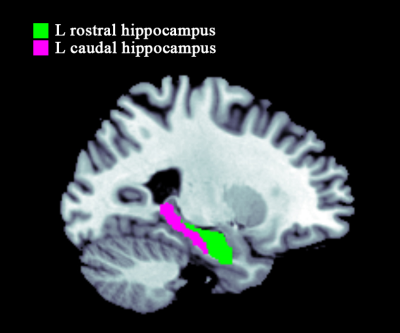
Four seeds of the hippocampus in the bilateral hemisphere. L
(R), left (right) hemisphere.
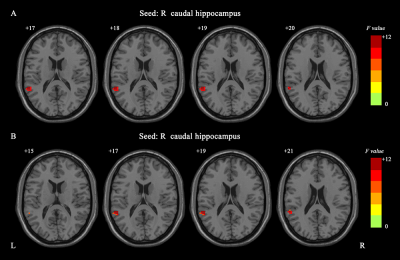
The significant dFC differences among the three groups for the
hippocampus seed (voxel p < 0.001,
cluster p < 0.05, GRF corrected).
The color bar indicates the F values
from One-Way ANOVA analyses. dFC, dynamic functional connectivity; GRF,
Gaussian random field; L (R), left (right) hemisphere.
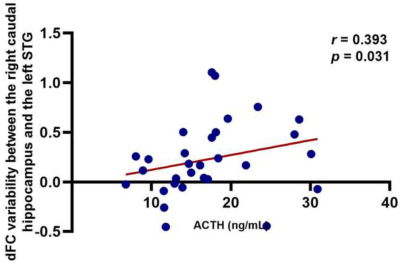
The correlations between significant dFC variability values and ACTH level in BDpatients with SA. BD, bipolar disorder; SA, suicide attempt; STG, superior temporal gyrus; ACTH: adrenocorticotropic hormone; L (R), left (right) hemisphere.
DOI: https://doi.org/10.58530/2023/1719