1711
Differentiation of brachial plexus caliber irregularities with simultaneous neurography and T2 mapping from MIXTURE1Department of Diagnostic Radiology and Radiation Oncology, Chiba Univerisity, Chiba, Japan, 2Department of Radiology, Chiba Univerisity Hospital, Chiba, Japan, 3Philips Japan, Tokyo, Japan
Synopsis
Keywords: Nerves, Neurography
Multifocal chronic inflammatory demyelinating polyneuropathy (CIDP) is characterized by asymmetrical and irregular nerve thickening. However, the nerves are sometimes irregular in caliber even without obvious neuropathy. MIXTURE can simultaneously acquire neurography and T2 mapping. The diameter and T2 values from MIXTURE were significantly wider and higher in multifocal CIDP than in cases with normal but irregular caliber (P = 0.029 and 0.004). The AUCs of ROC analyses were 0.889 and 0.972 in diameter and T2 values for differentiating the two groups. Diameter and T2 values acquired with MIXTURE help differentiate whether caliber irregularities in the brachial plexus are pathological.Introduction
MR neurography is used to evaluate peripheral nerve diseases. Chronic inflammatory demyelinating polyneuropathy (CIDP) shows thickening and increased signal on T2WI. CIDP is classified into typical CIDP and CIDP variants. CIDP variants include several subtypes, one of which is multifocal CIDP. Multifocal CIDP is characterized by heterogeneous peripheral nerve demyelination and irregular caliber 1. However, sometimes the nerves may be irregular in caliber even in the absence of obvious neuropathy, requiring differentiation from multifocal CIDP (Figure 1). In addition to diameter evaluation, T2 values have been reported to be useful in differentiating CIDP from healthy controls.Multi-Interleaved X-prepared tse with inTUitive RElaxometry (MIXTURE) can produce neurography and T2 mapping simultaneously. T2-mapping was performed using T2-prepared 3D segmented turbo spin-echo (TSE) with variable refocusing pulse trains. Two images with different TE (TE = 0 and 50ms) were acquired with interleaved acquisition. To obtain STIR contrast, inversion time (TI) was adjusted to suppress fat. The scheme of the MIXTURE is shown in Figure 2. In this study, we tried to differentiate multifocal CIDP from cases with irregular caliber but clinically normal by MIXTURE.
Methods
Consecutive112 cases who underwent MR neurography with MIXTURE from April 2021 to October 2022 were included in this study. The acquisition parameters of MIXTURE are shown in Figure 3. The patients diagnosed with multifocal CIDP based on the European Academy of Neurology/Peripheral Nerve Society guideline were included2. Next, patients with no abnormalities in the brachial plexus region were visually evaluated by a board-certified radiologist (17 years of experience), and those with irregularities in the caliber were included.The diameter and T2 values of the thickened area in the brachial plexus were measured in the multifocal CIDP and nerve irregularity but in normal cases. Analysis was used to evaluate the diagnostic performance of the diameter and T2 values. The two groups were compared using the Mann-Whitney test, with a P value of less than 0.05 considered significant. Receiver operating characteristic (ROC) analysis was used to evaluate the diagnostic performance of diameter and T2 values.
Results
Six multifocal CIDP patients were enrolled (age, 39.8±13.0; woman 4). Six of 41 (14.6%) normal cases in the brachial plexus showed nerve irregularity (age, 50.8±17.2; woman 0). There were no significant differences in age or gender (P = 0.240 and 0.109). The diameter of the thickened area was significantly wider in multifocal CIDP than in cases with normal but irregular caliber (P = 0.029, Figure 4A). T2 values were also significantly higher in multifocal CIDP (P = 0.004, Figure 4B). ROC analysis showed areas under the curve (AUC) for diameter and T2 values of 0.889 and 0.972, respectively (Figure 5).Discussion
Multifocal CIDP is the most common of CIDP variants, causing heterogeneous demyelination, and is often refractory to intravenous immunoglobulin used in typical CIDP. CIDP is known to cause nerve thickening and signal elevation on T2WI. Typical CIDP shows symmetrical and smooth thickening, whereas multifocal CIDP is known to cause asymmetrical and irregular nerve thickening. However, in clinical practice, irregular nerve caliber can be observed even in cases that are considered clinically normal. There are no reports of morphological and quantitative analysis of such cases.In the present study, we found significant differences in diameter and T2 values between multifocal CIDP and normal but with caliber irregularity. AUCs were high in ROC analysis, which may be useful for differentiation. The AUC of T2 value was higher than that of the diameter, which is in line with a report that T2 value has a higher AUC than the diameter for differentiating CIDP from normal control3,4. Although there have been many reports of diseases showing nerve thickening, there are still only a few reports, and the number of reports of MR neurography is expected to increase in the future. Therefore, it would be of clinical significance to clarify that even normal patients can present with caliber irregularities and their findings.
There are several limitations to this study. First, it is a small study. Although the number of cases was small, a clear and significant difference was obtained. Second, the study did not examine pathology. The possibility that small neurogenic tumors may be included cannot be excluded. However, a biopsy of the brachial plexus is clinically extremely difficult.
Conclusion
Diameter and T2 values acquired with MIXTURE are useful in differentiating whether caliber irregularities in the brachial plexus are pathological.Acknowledgements
No acknowledgement found.References
- Shibuya K, Sugiyama A, Ito S-I, Misawa S, Sekiguchi Y, Mitsuma S, Iwai Y, Watanabe K, Shimada H, Kawaguchi H, Suhara T, Yokota H, Matsumoto H, Kuwabara S. Reconstruction magnetic resonance neurography in chronic inflammatory demyelinating polyneuropathy. Ann Neurol 2015;77:333–337. 2.
- Van den Bergh PYK, van Doorn PA, Hadden RDM, Avau B, Vankrunkelsven P, Allen JA, Attarian S, Blomkwist-Markens PH, Cornblath DR, Eftimov F, Goedee HS, Harbo T, Kuwabara S, Lewis RA, Lunn MP, Nobile-Orazio E, Querol L, Rajabally YA, Sommer C, Topaloglu HA. European Academy of Neurology/Peripheral Nerve Society guideline on diagnosis and treatment of chronic inflammatory demyelinating polyradiculoneuropathy: Report of a joint Task Force-Second revision. J Peripher Nerv Syst 2021;26:242–268.
- Hiwatashi A, Togao O, Yamashita K, Kikuchi K, Momosaka D, Nakatake H, Yamasaki R, Ogata H, Yoneyama M, Kira J-I, Honda H. Lumbar plexus in patients with chronic inflammatory demyelinating polyradiculoneuropathy: evaluation with simultaneous T2 mapping and neurography method with SHINKEI. Br J Radiol 2018;91:20180501.
- Hiwatashi A, Togao O, Yamashita K, Kikuchi K, Momosaka D, Nakatake H, Yamasaki R, Ogata H, Yoneyama M, Kira J-I, Honda H. Simultaneous MR neurography and apparent T2 mapping in brachial plexus: Evaluation of patients with chronic inflammatory demyelinating polyradiculoneuropathy. Magn Reson Imaging 2019;55:112–117.
Figures
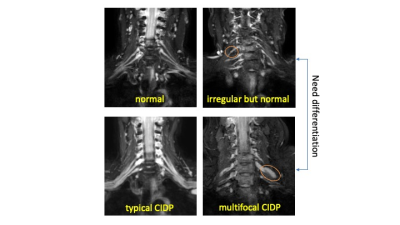
Figure 1. MR neurography of the brachial plexus
The nerve roots are thin and symmetrical in the normal case. Typical CIDP shows symmetrical and smooth nerve thickening. When nerve irregularity is revealed on MR neurography, it is necessary to differentiate between multifocal CIDP and clinically meaningless cases.
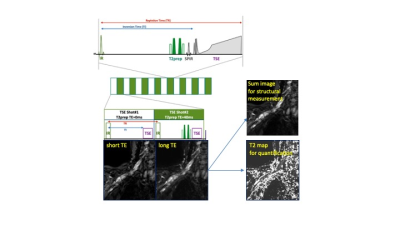
Figure 2. The schema of Multi-Interleaved X-prepared tse with inTUitive RElaxometry (MIXTURE)
MIXTURE can acquire images with short and long TE and can calculate T2 map. Sum images of short and long TE images give neurography with high contrast.
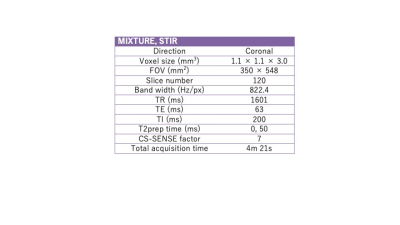
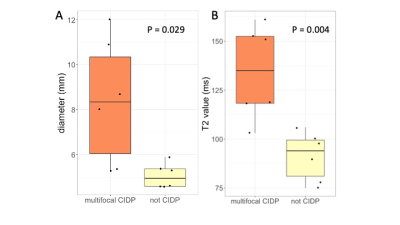
Figure 4. The box and jitter plots between multifocal CIDP and not-CIDP cases.
The diameter and T2 values of multifocal CIDP were significantly wider and higher in cases with normal but irregular caliber (P = 0.029 and 0.004).
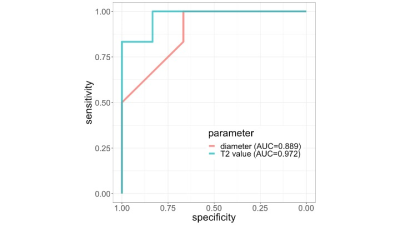
Figure 5. ROC curves of diameter and T2 value
AUCs for differentiating between multifocal CIDP and the cases with normal but irregular caliber were 0.889 and 0.972 in diameter and T2 values, respectively.