1686
Contrast-enhanced MRA with GRASP outperforms the conventional TWIST in aortic dissection patient cohort1DIPR (Department of Interventional and Pediatric Radiology), Inselspital, Bern, Switzerland, 2Department of Cardiovascular Surgery, Inselspital, Bern, Switzerland
Synopsis
Keywords: Vessels, Cardiovascular, Magnetic Resonance Angiography
This work compares the application of two magnetic resonance angiography (MRA) sequences on an aortic dissection patient cohort: the conventional cartesian-sampling-based, TWIST sequence, and the new radial-sampling-based GRASP sequence. The 1.5T MRA data from six patients with aortic dissection were assessed qualitatively and quantitatively to investigate overall image quality and spatial and temporal blurring. GRASP outperformed TWIST in temporal SNR, vessel sharpness and reduction in image blurring; streaking artifacts were clearly visible, but did not affect the diagnostic image quality.Introduction
Gadolinium-based contrast-enhanced time-resolved magnetic resonance angiography (CE-MRA) techniques are able to depict the anatomy and dynamics of complex vascular structures [1]. This is desirable in order to reduce the number of invasive procedures with their inherent radiation exposure for patients who otherwise may undergo repetitive X-ray angiograms during follow-up. Time-resolved angiography With Interleaved Stochastic Trajectories (TWIST) sequence is conventionally used to perform a time-resolved 3D CE-MRA; it is based on Cartesian acquisition and sharing of k-space data between adjacent time frames [2]. This trajectory is prone to respiratory-motion-induced image artefacts, such as spatial blurring of vascular boundaries. Radial-sampling-based techniques, such as GRASP (Golden-angle radial sparse parallel) MRI sequence, are less sensitive to motion than cartesian sampling, and consequently improve the overall image quality [3]. So far, GRASP is used in clinical routine to acquire contrast-enhanced liver dynamics. In this work we aim to qualitatively and quantitatively compare the performance of TWIST and GRASP for time-resolved CE-MRA on patients with aortic dissection.Methods
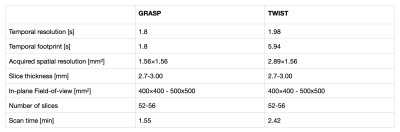
A cohort of six patients (55±9.48y.o., one female) with aortic dissection underwent a clinical routine examination including a TWIST and a GRASP sequences (acquisition parameters are summarised in Table 1). Prior each CE-MRA acquisitions the same amount of Gadovist-contrast-agent (Bayer, Switzerland AG Zurich) was administered (0.075ml/kg, flow 4ml/s). Both sequences were acquired in reverse order for half of the patients, with a three-minutes-pause between the contrast administrations. All data were acquired on a 1.5T Magnetom SolaFit scanner equipped with a 32 channel body coil (Siemens, Erlangen). An experienced radiologist assessed the overall image quality, contrast, vessel sharpness and image artefacts by grading the images as follows: 1=excellent; 2=acceptable; 3=poor; 4=non-diagnostic. To perform quantitative image analysis, circular regions-of-interest (ROIs) were placed at three aorta levels: ascending aorta (AA), descending aorta at the level of the pulmonary trunk (DA pulm), and descending aorta at the level of the infrarenal arteries (DA renal). Maximum slope of the contrast agent uptake and the full width at half maximum (FWHM) were calculated from the normalized signal intensity time courses in the ROIs. To analyse spatial blurring, vessel sharpness was calculated from the intensity profiles at the same levels in the aorta [4]. Additionally, temporal signal-to-noise ratio (tSNR) was calculated from the second half of the time course after the first pass bolus passage.Results
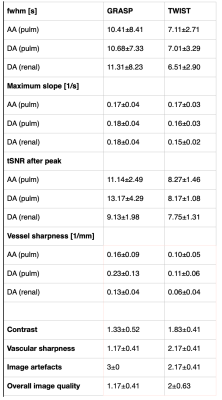
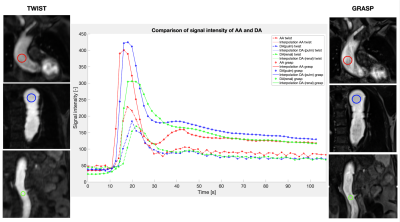
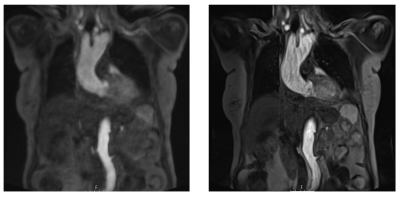
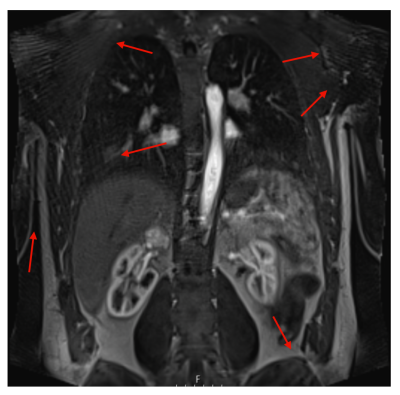
The results of the quantitative and qualitative assessment are summarised in Table 2: GRASP was superior in tSNR, soft tissue contrast, vessel sharpness, and the overall image quality, TWIST was superior in FWHM, and lower artifact levels. Maximum upslope is similar. Figure 1 shows the signal intensities over time for AA (red), DA at the levels of pulmonary trunk (blue) and infrarenal arteries (green) for GRASP and TWIST: with the current acquisition and reconstruction parameters, the absolute signal of GRASP is clearly higher than TWIST and corresponding time-courses are smoother. Representative images of TWIST and GRASP are in Figure 2: one can see a superior soft tissue contrast and a better impression regarding image sharpness. Streaking artefacts of GRASP are in Figure 3.Discussion
The GRASP sequence provided a superior overall image quality index, resulting from the qualitative scores of soft tissue contrast, sharpness and artifact level – despite an increased artifact level compared to TWIST. The level of streaking artifacts can increase with the level of undersampling, i.e. when the number of acquired spokes is reduced. However, most streaking artifacts appeared in the periphery of the field-of-view (FOV) and the images remained of diagnostic value in the aortic regions. The improved vessel sharpness, both qualitative and quantitative, for all ROIs in GRASP compared to TWIST is assumed to result from the higher in-plane resolution and from reduced sensitivity of the radial trajectory to respiratory motion. The higher levels of tSNR in GRASP data compared to TWIST data (also visible in smoother signal-time-courses in Figure 1) in all locations of the aorta are likely linked to the smaller temporal footprint (temporal resolution). In TWIST, k-space lines are taken from a wider time range to reconstruct a single time frame resulting in a temporal footprint three times higher than temporal resolution (based on k-space center A=25% and sampling density of k-space periphery B=33%) [2]. Contrary, the FWHM was lower for TWIST in all locations indicating the weighting of the k-space center for the image contrast in TWIST (scan time for A~1s). It is possible to improve FWHM of GRASP by taking fewer radial projections to reconstruct a single time frame, but this may come at the cost of increased radial undersampling artifacts.Conclusion
In this proof-of-the-concept study, CE-MRA with GRASP has allowed us to acquire qualitatively better data compared to TWIST. Including GRASP in the clinical protocols may improve diagnosis of aortic dissection patients in future. However, more data sets need to be evaluated to allow for statistical considerations. Furthermore, it is of interest to investigate the number of spokes used for the calculation of a time frame on the impact of contrast dynamics and artifact level in more detail.Acknowledgements
This study was funded by the Swiss National Foundation, Synergia CRSII5_193694. We thank the MR Team (Andrina Auderset, Anja Bassi, Luuk Arjan Gottemaker, Sophie Monney, Albert Muhaxheri, Catia Nunes Barros de Jesus, Flavia Schranz, Tamara Schürch) and Grazia Maria Cereghetti.
References
[1] Grist TM et al. Time-resolved angiography: Past, present, and future. J Magn Reson Imaging 2012;36:1273-86.
[2] Laub G. Kroeker R. syngo TWIST for dynamic time-resolved MR angiography. MAGNETOM Flash 2006;3;92-95.
[3] Feng L et al. Golden-angle radial sparse parallel MRI: combination of compressed sensing, parallel imaging, and golden-angle radial sampling for fast and flexible dynamic volumetric MRI. Magn Reson Med 2014;72:707-17.
[4] Larson AC, Kellman P, Arai A, et al. Preliminary investigation of respiratory self-gating for free-breathing segmented cineMRI. Magn Reson Med 2005;53:159-168.
Figures